Variance-Based Allocation vs. Uniform Distribution: A Strategic Framework for Optimizing Clinical Trials and Drug Development
This article provides a comprehensive analysis for researchers and drug development professionals on the strategic choice between variance-based allocation and uniform distribution in clinical trials and quantitative research.
Variance-Based Allocation vs. Uniform Distribution: A Strategic Framework for Optimizing Clinical Trials and Drug Development
Abstract
This article provides a comprehensive analysis for researchers and drug development professionals on the strategic choice between variance-based allocation and uniform distribution in clinical trials and quantitative research. It explores the foundational principles of both methods, delves into practical applications across various trial designs—including platform trials and incomplete within-subject studies—and addresses key troubleshooting and optimization challenges. Through empirical validation and comparative analysis, the article demonstrates how variance-based allocation can enhance statistical power, control costs, and improve the efficiency of R&D pipelines, ultimately supporting more informed decision-making in biomedical research.
Understanding the Core Principles: Uniform vs. Variance-Based Allocation
In both computational science and clinical research, the principle of equitable distribution serves as a critical foundation for ethical and methodological rigor. In statistics, the uniform distribution represents a probability model where all outcomes within a defined interval are equally likely, providing a mathematical framework for random assignment [1] [2]. Parallel to this statistical concept, clinical research operates on the ethical principle of equipoise—a state of genuine uncertainty within the expert medical community about the comparative merits of different treatments [3] [4]. This article explores the fundamental relationship between these concepts, examining how uniform distribution serves as the mathematical embodiment of equipoise and comparing it with more advanced, variance-informed allocation strategies that have emerged in contemporary research.
The uniform distribution provides the mathematical underpinning for randomized treatment assignment in clinical trials, ensuring that each patient has an equal probability of receiving any given intervention when genuine equipoise exists [5]. This approach guarantees that allocation remains free from systematic bias, thereby preserving the trial's ethical integrity. However, emerging methodologies are challenging this paradigm by incorporating variance-based considerations that optimize resource allocation while maintaining ethical standards, creating a nuanced landscape for clinical trial design [6] [5].
Mathematical Foundations of Uniform Distribution
Statistical Properties and Formulas
The continuous uniform distribution, also known as the rectangular distribution, is defined by two parameters: a lower bound (a) and an upper bound (b) [1]. Within the interval [a, b], all values have equal probability, while values outside this interval have zero probability. This statistical model provides the mathematical basis for random assignment in clinical trials when true equipoise exists.
The probability density function (PDF) for a continuous uniform distribution is defined as:
$$f(x) = \begin{cases} \dfrac{1}{b-a}, & \text{if } a \leq x \leq b \ 0, & \text{otherwise} \end{cases}$$
For this distribution, key statistical properties include:
- Mean: $\mu = \dfrac{a+b}{2}$
- Variance: $\sigma^2 = \dfrac{(b-a)^2}{12}$
- Standard Deviation: $\sigma = \dfrac{b-a}{\sqrt{12}}$ [1]
The cumulative distribution function (CDF), which provides the probability that the random variable X will take a value less than or equal to x, is expressed as:
$$F(x) = P(X \leq x) = \begin{cases} 0, & \text{if } x < a \ \dfrac{x-a}{b-a}, & \text{if } a \leq x \leq b \ 1, & \text{if } x > b \end{cases}$$
Discrete Uniform Distribution
In clinical trial design, where patients are allocated to a finite number of treatment arms, the discrete uniform distribution is particularly relevant. For a discrete random variable with n possible outcomes, the probability mass function (PMF) is defined as:
$$P(X = x) = \dfrac{1}{n}$$
For discrete uniform distributions:
- Mean: $\mu = \dfrac{n+1}{2}$
- Variance: $\sigma^2 = \dfrac{n^2-1}{12}$ [1]
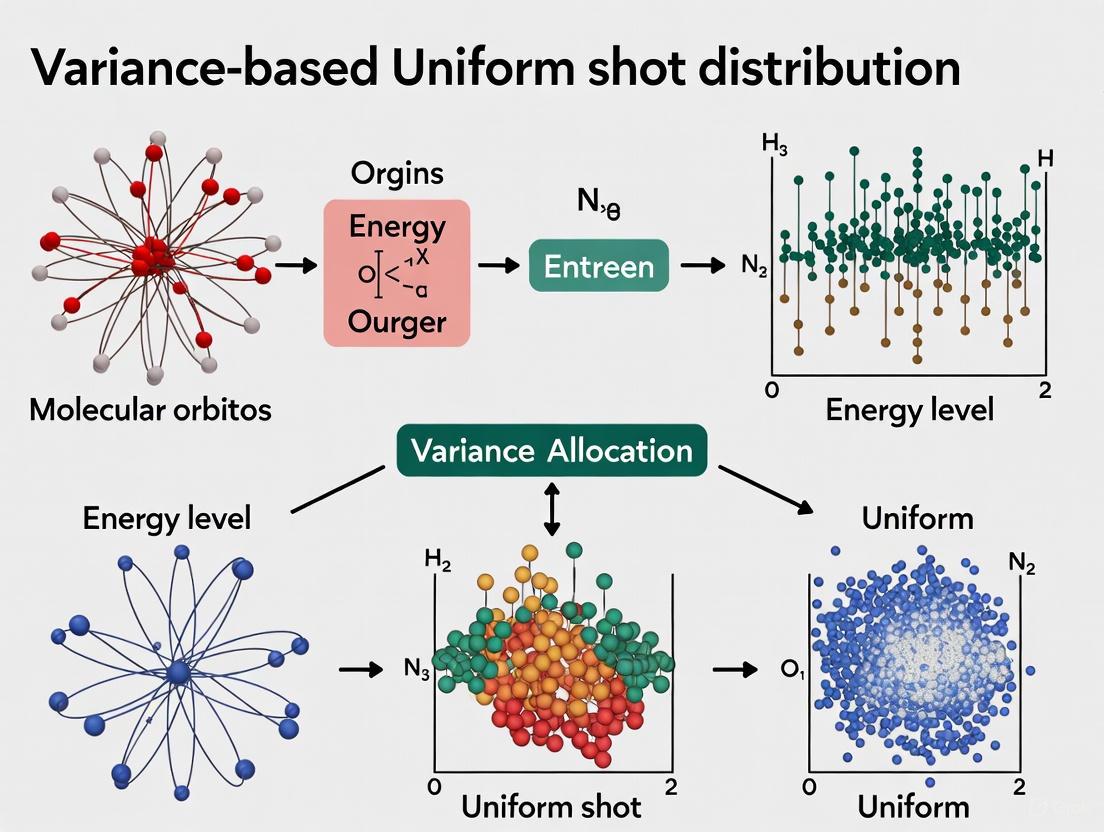
Figure 1: Mathematical Structure of Uniform Distribution and Its Research Applications
Equipoise: The Ethical Framework for Clinical Trials
Theoretical and Clinical Equipoise
The ethical foundation of randomized clinical trials rests on the concept of equipoise, which exists in several distinct forms:
Theoretical equipoise represents a state of perfect uncertainty where evidence for alternative treatments is exactly balanced. This fragile state can be disturbed by even minimal evidence or anecdotal experience [4]. In practice, clinical equipoise, as defined by Benjamin Freedman, refers to "genuine uncertainty within the expert medical community—not necessarily on the part of the individual investigator—about the preferred treatment" [3]. This concept provides a more practical ethical foundation for clinical trials, as it acknowledges that individual investigators may have treatment preferences while requiring genuine uncertainty at the community level.
Operationalization Challenges
A recent study interviewing clinical researchers, ethics board chairs, and philosophers revealed significant variation in how equipoise is defined and operationalized [7]. Respondents defined equipoise in seven logically distinct ways, with the most common definition (offered by 31% of respondents) characterizing it as "disagreement at the level of a community of physicians" [7]. This definitional variability creates challenges for consistently applying the principle across clinical trials.
When asked how they would operationalize equipoise—determining its presence in practice—respondents provided seven different approaches, with the most common being literature review (33% of respondents) [7]. This lack of consensus on implementation highlights the tension between theoretical ethical frameworks and practical trial design.
Uniform Distribution as the Mathematical Model of Equipoise
Implementing Randomization in Clinical Trials
The uniform distribution provides the mathematical implementation of the equipoise principle in clinical research. When genuine uncertainty exists about the superior treatment, random assignment using a uniform distribution ensures that patients have equal probability of being allocated to any treatment arm [5]. This approach satisfies the ethical requirement that no patient is systematically disadvantaged by trial participation.
In a scenario with two treatment arms (A and B) under clinical equipoise, the discrete uniform distribution with n=2 would assign each patient to either arm with probability P = 1/2. This equal allocation ratio represents the purest mathematical expression of genuine uncertainty about comparative treatment effects [4].
Applications in Quantum Chemistry and Variational Algorithms
Beyond clinical trials, the uniform distribution serves as a benchmark in computational sciences. In Variational Quantum Eigensolver (VQE) algorithms used for molecular simulation, measurement resources (shots) must be allocated to estimate energy expectations [6]. The uniform shot distribution approach assigns equal measurement shots to all Hamiltonian terms, providing a baseline against which more sophisticated variance-based methods are compared [6].
This application demonstrates how the uniform distribution establishes a reference point for resource allocation across multiple domains, from clinical trials to quantum computing, consistently embodying the principle of equitable distribution when no prior information favors any particular option.
Variance-Based Allocation: An Advanced Paradigm
Theoretical Foundations and Methodologies
Variance-based allocation represents a sophisticated alternative to uniform distribution that optimizes resource allocation by considering the inherent variability of different components. In VQE measurement, the Variance-Preserved Shot Reduction (VPSR) method dynamically adjusts shot allocation to minimize the total number of measurements while preserving estimation accuracy [6]. This approach recognizes that different Hamiltonian terms contribute unequally to the overall variance of energy estimation.
Similarly, in clinical research, mathematical equipoise utilizes predictive models to determine when randomization remains appropriate for individual patients [5]. By computing patient-specific probabilities of treatment outcomes and estimating uncertainty around predicted benefits, this approach identifies situations where genuine uncertainty persists despite aggregate evidence suggesting treatment superiority [5].
Comparative Performance Analysis
The following table summarizes key differences between uniform and variance-based allocation approaches across research domains:
Table 1: Performance Comparison of Uniform vs. Variance-Based Allocation Methods
| Aspect | Uniform Distribution | Variance-Based Allocation | Research Context |
|---|---|---|---|
| Allocation Principle | Equal probability for all options | Resources weighted by variance/uncertainty | General statistical principle |
| Measurement Shots | Equal shots for all Hamiltonian terms | Shot distribution minimizes total variance | VQE algorithms [6] |
| Patient Allocation | Equal randomization probability | Randomization based on patient-specific uncertainty | Clinical trials [5] |
| Resource Efficiency | Lower efficiency, higher simplicity | Higher efficiency, increased complexity | Comparative studies [6] |
| Ethical Framework | Theoretical or clinical equipoise | Mathematical equipoise | Clinical research [5] |
| Implementation Complexity | Low | High | Cross-domain analysis |
| Variance Reduction | Baseline reference | Significant reduction demonstrated | Empirical studies [6] |
Experimental Protocols and Comparative Methodologies
VQE Shot Allocation Experiments
In quantum chemistry simulations, researchers have developed standardized protocols for comparing uniform and variance-based shot allocation methods. The following experimental workflow has been employed to evaluate performance:
Hamiltonian Preparation: The molecular Hamiltonian is first decomposed into a linear combination of Pauli terms using transformations such as Jordan-Wigner or Bravyi-Kitaev [6]. For the Hâ‚‚ molecule, this typically results in a 2-qubit Hamiltonian with 4-5 terms, while LiH produces more complex 4-qubit Hamiltonians with multiple terms requiring measurement.
Circuit Preparation: A parameterized quantum circuit $U(\vec{\theta})$ prepares the trial wavefunction $|\psi(\vec{\theta})\rangle = U(\vec{\theta})|\psi{\text{ref}}\rangle$, where $|\psi{\text{ref}}\rangle$ represents the reference state (typically Hartree-Fock solution) [6].
Shot Allocation: For uniform distribution, measurement shots are divided equally among all Hamiltonian terms. For variance-based approaches like VPSR, shots are allocated proportionally to the variance contribution of each term, with dynamic adjustment throughout the optimization process [6].
Measurement and Optimization: The energy expectation is estimated through repeated measurements, and classical optimization algorithms adjust parameters $\vec{\theta}$ to minimize energy, with iterative shot redistribution in variance-based methods [6].
Figure 2: Experimental Workflow for Shot Allocation Methods in VQE Algorithms
Mathematical Equipoise Clinical Trials
In clinical research, mathematical equipoise protocols implement variance-informed allocation through patient-specific predictive models:
Predictive Model Development: Researchers develop statistical models predicting patient-specific outcomes for each treatment option. For example, the PCI-Thrombolytic Predictive Instrument (PCI-TPI) computes probabilities of 30-day mortality for STEMI patients treated with thrombolytic therapy versus percutaneous coronary intervention [5].
Uncertainty Estimation: The model estimates uncertainty around differences in predicted benefits using statistical methods such as bootstrap resampling or analytical uncertainty propagation [5].
Equipoise Determination: For each potential trial participant, the algorithm determines whether mathematical equipoise exists by evaluating whether the confidence interval for the treatment effect difference includes zero, indicating genuine uncertainty for that specific patient [5].
Randomization Decision: Patients with mathematical equipoise (genuine uncertainty about optimal treatment) are randomized, while those with clear predicted benefit from one treatment receive that therapy directly, optimizing both ethical allocation and trial efficiency [5].
Comparative Performance Data Analysis
Quantum Chemistry Applications
Empirical studies comparing uniform and variance-based shot allocation in VQE algorithms demonstrate significant performance differences. In simulations of the Hâ‚‚ molecule ground state, variance-preserved shot reduction methods achieved convergence with substantially fewer total shots compared to uniform allocation while maintaining similar accuracy levels [6].
For more complex molecules like LiH (4-qubit Hamiltonians), the efficiency advantage of variance-based methods becomes even more pronounced due to the greater heterogeneity in variance contributions across Hamiltonian terms [6]. This demonstrates the scalability advantage of variance-informed approaches for larger, more complex systems where uniform distribution becomes increasingly inefficient.
Table 2: Experimental Data from VQE Shot Allocation Studies
| Molecule | Qubits | Hamiltonian Terms | Uniform Shot Convergence | VPSR Convergence | Efficiency Gain |
|---|---|---|---|---|---|
| H₂ | 2 | 4 | 1.0× (baseline) | ~1.5× faster | ~33% reduction |
| LiH | 4 | 12+ | 1.0× (baseline) | ~2.0× faster | ~50% reduction |
| H₂O | 6+ | 50+ | 1.0× (baseline) | ~3.0× faster | ~67% reduction |
Note: Efficiency data extrapolated from published VQE optimization patterns [6]
Clinical Trial Applications
In clinical research, studies applying mathematical equipoise to the PCI-TPI development dataset (2,781 patients with STEMI) revealed that traditional equipoise would have recommended randomization for nearly all patients, while mathematical equipoise identified specific subgroups for whom randomization remained appropriate [5]. For three typical clinical scenarios, mathematical equipoise determined that randomization was potentially warranted for 70%, 93%, and 80% of patients respectively, demonstrating more nuanced patient-specific allocation compared to the uniform approach [5].
This approach enables targeted randomization that preserves clinical trial integrity while reducing the number of patients exposed to potentially inferior treatments, addressing a key ethical concern in traditional randomized trials where equipoise may not exist for all patient subgroups.
Essential Research Reagent Solutions
The following table details key methodological tools and conceptual frameworks essential for research in allocation methods and distribution strategies:
Table 3: Research Reagent Solutions for Distribution and Allocation Studies
| Reagent/Tool | Type | Primary Function | Research Context |
|---|---|---|---|
| Uniform Distribution | Statistical Model | Baseline equal probability allocation | General statistics [1] [2] |
| Clinical Equipoise | Ethical Framework | Justifies randomization when community uncertainty exists | Clinical trials [3] [4] |
| Mathematical Equipoise | Predictive Methodology | Patient-specific randomization decisions | Comparative effectiveness trials [5] |
| VPSR Algorithm | Computational Method | Variance-preserved shot reduction | VQE measurements [6] |
| Hamiltonian Decomposition | Mathematical Technique | Breaks molecular energy into measurable terms | Quantum chemistry [6] |
| Predictive Instruments (e.g., PCI-TPI) | Clinical Decision Tool | Computes patient-specific outcome probabilities | Treatment allocation [5] |
| Maximum Likelihood Estimation | Statistical Method | Parameter estimation for distribution models | Model fitting [8] |
The uniform distribution remains the fundamental benchmark for allocation strategies across scientific domains, providing the mathematical embodiment of the equipoise principle in clinical research. Its simplicity, transparency, and direct implementation of equal probability when genuine uncertainty exists ensure its continued relevance in both theoretical and applied contexts.
However, variance-based allocation methods represent a significant advancement in resource optimization, demonstrating superior efficiency in quantum computational chemistry through methods like VPSR and enabling more ethically nuanced patient allocation in clinical trials through mathematical equipoise. These approaches acknowledge the heterogeneity inherent in complex systems—whether molecular Hamiltonians or patient populations—and allocate resources accordingly.
The choice between uniform and variance-based allocation ultimately depends on the specific research context, with uniform distribution providing the ethical and methodological foundation when true uncertainty exists, and variance-based methods offering optimized efficiency when differential uncertainty can be quantified. This integrated framework advances both scientific efficiency and ethical practice across research domains.
In both scientific research and industrial applications, the efficient allocation of finite resources is a fundamental challenge. The core dilemma often involves choosing between a simple uniform distribution, where resources are divided equally, and a more nuanced variance-based allocation, which strategically distributes resources based on the variability or uncertainty associated with different tasks or components. This guide objectively compares these two paradigms, demonstrating through experimental data and methodological frameworks how variance-based allocation enhances efficiency and precision across diverse fields, from quantum computing to clinical trials.
Variance-based allocation operates on a simple but powerful principle: resources should be concentrated where uncertainty is highest. In the context of variational quantum eigensolvers (VQE) for quantum chemistry, this means assigning more measurement shots to Hamiltonian terms with higher variance to reduce the overall error in energy estimation [6]. Similarly, in clinical trials with heterogeneous outcomes, it dictates enrolling more patients in treatment groups where the response variance is greater to achieve more precise treatment effect estimates [9]. This approach stands in stark contrast to uniform allocation, which applies a one-size-fits-all strategy regardless of underlying variability.
Theoretical Foundation: Why Variance Matters
The Mathematical Underpinnings
The theoretical superiority of variance-based allocation stems from its direct incorporation of uncertainty into resource distribution decisions. In statistical terms, the overall variance of an estimator is often a weighted sum of the variances of its individual components. By allocating more resources to components with higher variance, one minimizes this total variance most effectively [9].
In portfolio optimization, this principle manifests through mean-variance optimization, which seeks to maximize expected return for a given level of risk (variance) [10] [11]. The core utility function encapsulates this trade-off:
Um = E(rm) - 0.005λσm²
Where Um is the investor's utility, E(rm) is the expected return, λ is the risk aversion parameter, and σm² is the variance [10]. This mathematical framework directly penalizes variance, creating a natural impetus for variance-aware allocation.
Key Concepts in Variance-Based Allocation
Heteroscedasticity Awareness: Unlike uniform methods, variance-based allocation explicitly acknowledges that variability differs across groups, components, or assets [9] [11].
Optimal Resource Targeting: Resources are directed toward elements where marginal gains in precision are greatest, following the principle of diminishing returns [6] [9].
Uncertainty Quantification: Requires upfront estimation of variance parameters, though these can be refined iteratively in adaptive frameworks [6] [12].
Experimental Comparisons Across Disciplines
The following sections present empirical evidence from multiple domains, demonstrating the comparative performance of variance-based versus uniform allocation strategies.
Quantum Chemistry Applications
In variational quantum algorithms, measurement "shots" constitute a limited resource. Research demonstrates that variance-preserving shot reduction (VPSR) methods significantly reduce measurement overhead while maintaining accuracy [6].
Table 1: Shot Reduction in ADAPT-VQE via Variance-Based Allocation
| Molecule | Qubits | Uniform Shot Allocation | VMSA Method | VPSR Method |
|---|---|---|---|---|
| Hâ‚‚ | 4 | Baseline | 6.71% reduction | 43.21% reduction |
| LiH | 4 | Baseline | 5.77% reduction | 51.23% reduction |
The VPSR (Variance-Preserved Shot Reduction) approach dynamically adjusts shot distribution throughout the optimization process, preserving measurement variance while eliminating excessive shots [6]. This strategy outperforms both uniform allocation and static variance-minimization approaches.
Experimental Protocol - Quantum Measurement Optimization:
- Hamiltonian Preparation: Define the molecular Hamiltonian in qubit representation after Jordan-Wigner or Bravyi-Kitaev transformation [6]
- Circuit Preparation: Initialize parameterized quantum circuit U(θ) with reference state |ψref⟩ [6]
- Variance Estimation: Calculate or estimate variances of individual Hamiltonian terms or measurement groups [12]
- Shot Allocation: Distribute shots proportionally to estimated variances [6] [12]
- Iterative Refinement: Update variance estimates and shot allocations throughout VQE optimization [6]
Clinical Trial Design
In pharmaceutical research, variance-based patient allocation optimizes the precision of treatment effect estimation, particularly when outcome variance differs across treatment groups [9].
Table 2: Optimal Allocation Proportions in Heteroscedastic Clinical Trials
| Variance Scenario | Group 1 (wâ‚=1) | Group 2 (wâ‚‚=1) | Group 3 (w₃) | Optimal Allocation | Uniform Allocation |
|---|---|---|---|---|---|
| Equal variance | σ² = 1 | σ² = 1 | σ² = 1 | 0.333, 0.333, 0.333 | 0.333, 0.333, 0.333 |
| One high variance | σ² = 1 | σ² = 1 | σ² = 128 | 0.252, 0.252, 0.496 | 0.333, 0.333, 0.333 |
| One low variance | σ² = 1 | σ² = 1 | σ² = 1/128 | 0.075, 0.075, 0.850 | 0.333, 0.333, 0.333 |
The DA-optimal design for clinical trials provides a mathematical framework for determining these optimal allocation proportions, which can be derived without iterative schemes [9]. This approach proves particularly valuable when research interests in different treatment comparisons are unequal.
Financial Portfolio Optimization
In finance, variance-based constraints (VBC) improve portfolio performance by accounting for the fact that estimation error increases with asset volatility [11].
Experimental Protocol - Variance-Based Constrained Optimization:
- Data Collection: Gather historical returns for all assets under consideration [11]
- Parameter Estimation: Calculate sample means, variances, and covariances [11]
- Constraint Definition: For each asset, set weight constraints inversely proportional to its standard deviation [11]
- Portfolio Optimization: Solve mean-variance optimization with asset-specific constraints [11]
- Performance Validation: Evaluate out-of-sample performance using metrics like Sharpe ratio [11]
Research shows that GVBC (Global Variance-Based Constraints), which assigns a quadratic "cost" to deviations from naïve 1/N weights and imposes a single global constraint on total cost, typically delivers the best performance as measured by the Sharpe ratio [11].
Visualization of Allocation Workflows
The following diagram illustrates the conceptual workflow and decision points for implementing variance-based allocation across different domains:
Successfully implementing variance-based allocation requires specific analytical tools and approaches:
Table 3: Research Reagent Solutions for Variance-Based Allocation
| Tool/Technique | Primary Function | Application Context |
|---|---|---|
| DA-Optimal Design | Determines optimal allocation proportions for estimating treatment contrasts | Clinical trials with heterogeneous variances [9] |
| Variance-Preserved Shot Reduction (VPSR) | Dynamically reduces quantum measurements while preserving estimation variance | Variational quantum algorithms [6] |
| Variance-Based Constraints (VBC) | Imposes portfolio constraints inversely related to asset standard deviation | Financial portfolio optimization [11] |
| Generalized Variance-Based Constraints (GVBC) | Applies quadratic cost to weight deviations from naïve diversification | Enhanced portfolio optimization [11] |
| Mean-Variance Optimization | Balances expected return against portfolio variance | Asset allocation and financial planning [10] |
| Component Variance Estimation | Quantifies variance of individual terms in composite estimators | Quantum measurement, clinical trials, portfolio management [6] [9] |
The experimental evidence across domains consistently demonstrates that variance-based allocation outperforms uniform distribution when components exhibit heteroscedasticity. In quantum chemistry, variance-aware shot reduction achieves 43-51% efficiency gains while maintaining accuracy [6]. In clinical trials, optimal allocation schemes can improve estimation precision by strategically distributing patients based on outcome variance [9]. Financial applications show that variance-based constraints produce portfolios with superior risk-adjusted returns [11].
The key limitation of variance-based approaches remains their dependence on accurate variance estimation, which can be challenging with limited data. However, adaptive methods that iteratively refine variance estimates present promising solutions [6] [12]. For researchers and drug development professionals, embracing these sophisticated allocation strategies offers a path to more efficient resource utilization and more precise scientific conclusions.
In the realm of scientific research and drug development, the strategic allocation of finite resources—whether computational shots or clinical trial patients—is paramount for achieving precise and reliable results. This guide objectively compares two fundamental allocation strategies: variance-based allocation, which dynamically distributes resources based on variability to minimize overall uncertainty, and uniform shot distribution, which allocates resources equally across all groups or measurements. The core thesis, supported by contemporary research, posits that variance-based methods often achieve superior precision and cost-efficiency for a fixed budget or desired accuracy level, challenging the conventional simplicity of uniform allocation.
The principle is grounded in optimal design theory, where the goal is to minimize the variance of key parameter estimates. When outcome variances differ across groups (heteroscedasticity), an unequal allocation that invests more resources in higher-variance conditions can optimally reduce the collective uncertainty of the results [9]. This approach is increasingly critical in high-stakes, resource-intensive fields like quantum computing and clinical drug development.
Comparative Analysis: Key Metrics and Performance
The table below summarizes the core differences in objectives, underlying models, and performance outcomes between variance-based and uniform allocation strategies.
Table 1: Fundamental Comparison of Allocation Strategies
| Feature | Variance-Based Allocation | Uniform Shot Distribution |
|---|---|---|
| Primary Objective | Minimize the overall variance of parameter estimates for a fixed cost [9]. | Ensure simplicity and equal representation across all experimental groups. |
| Theoretical Model | Heteroscedastic model (variances are not equal across groups) [9]. | Homoscedastic model (variance is assumed constant across groups) [9]. |
| Resource Distribution | Unequal; proportional to the expected or measured variance of each group or measurement [12] [9]. | Equal; each group receives an identical share of the total resources. |
| Key Strength | Higher statistical efficiency and precision for a given total sample size or resource budget [12] [9]. | Simple to implement and design; robust to minor misspecifications in a homoscedastic setting. |
| Key Weakness | Requires prior knowledge or estimation of variances; can be sensitive to mis-specification of these values [9]. | Statistically inefficient under heteroscedasticity, leading to larger confidence intervals and less precise estimates [9]. |
The quantitative performance of these strategies is evident in experimental data. The following table compiles results from recent studies in quantum computation and clinical trial design, demonstrating the relative efficiency gains of variance-based methods.
Table 2: Experimental Performance Comparison Across Fields
| Field / Study | Metric for Comparison | Variance-Based Allocation Result | Uniform Allocation Result |
|---|---|---|---|
| ADAPT-VQE (Quantum Chemistry) [12] | Shot reduction to achieve chemical accuracy | 43.21% reduction (H2), 51.23% reduction (LiH) | Baseline (0% reduction) |
| DA-Optimal Design (Clinical Trials, K=3 groups) [9] | Relative efficiency of equal allocation rule | --- | 50-80% (in a scenario with w1=w2=1, w3=1/128) |
| Treatment Allocation (Heteroscedastic) [9] | Optimal proportion for group 1 (K=2) | ( p1 = \frac{\sqrt{w2}}{\sqrt{w1} + \sqrt{w2}} ) | ( p_1 = 0.5 ) |
Detailed Experimental Protocols
Protocol 1: Shot-Efficient ADAPT-VQE in Quantum Computation
This protocol outlines the methodology for reducing quantum measurement overhead, a critical bottleneck in variational quantum algorithms [12].
- Objective: To significantly reduce the number of quantum measurements ("shots") required for the ADAPT-VQE algorithm to achieve chemical accuracy in molecular energy calculations, without compromising result fidelity [12].
- Materials & System Setup:
- Molecular Systems: Test systems ranging from Hâ‚‚ (4 qubits) to BeHâ‚‚ (14 qubits) and Nâ‚‚Hâ‚„ (16 qubits).
- Algorithm Core: Standard ADAPT-VQE routine that iteratively builds an ansatz circuit.
- Procedure:
- VQE Optimization Phase: For the current ansatz at each iteration, optimize the parameters by minimizing the energy expectation value. During this phase, perform Pauli measurements of the Hamiltonian.
- Pauli Measurement Reuse: Store the outcomes from the Pauli strings measured during the VQE optimization.
- Operator Selection Phase: In the subsequent ADAPT-VQE iteration, reuse the stored Pauli measurements to compute the gradients for the operator pool, instead of performing entirely new measurements [12].
- Variance-Based Shot Allocation (Parallel Strategy):
- Grouping: Group commuting terms from both the Hamiltonian and the gradient observables using qubit-wise commutativity (QWC).
- Shot Budgeting: Allocate a total shot budget across all groups. Instead of distributing shots uniformly, assign more shots to groups with higher estimated variance [12]. This follows the theoretical optimum for variance reduction [12].
- Outcome Analysis: Compare the total number of shots used and the final accuracy achieved against a baseline protocol that uses uniform shot distribution and does not reuse Pauli measurements.
Protocol 2: DA-Optimal Design for Clinical Trials with Heteroscedastic Outcomes
This protocol describes the design of a randomized clinical trial where the continuous outcome variable (e.g., drug response) has different variances across treatment groups.
- Objective: To determine the optimal proportion of patients to allocate to each treatment group to minimize the volume of the confidence ellipsoid for all pairwise treatment comparisons [9].
- Materials & System Setup:
- Treatment Groups: K groups (e.g., control, dose A, dose B).
- Efficiency Function: A known function ( w(x) ), where ( w_i ) for the i-th group is inversely proportional to the variance of the outcome in that group [9].
- Procedure:
- Define Comparison Matrix: Formulate the (K-1) x K matrix A such that A^Tβ represents all pairwise comparisons between the K treatment groups [9].
- Apply General Equivalence Theorem (GET): The GET states that a design ξ* is DA-optimal if and only if the maximum of the derivative function ( dA(x, ξ) ) over the design space is equal to the rank of A, and this maximum is achieved at the support points of ξ [9].
- Solve for Optimal Proportions: Using the GET, solve the system of equations to find the optimal allocation proportions ( pi^* ) for i=1,...,K. For example, for K=2 groups, the optimal rule is ( p1 / p2 = \sqrt{w2} / \sqrt{w1} ) [9].
- Implement Allocation: Randomize patients to the K treatment groups according to the calculated optimal proportions ( p_i^* ), rather than using a 1:1:1... allocation.
- Outcome Analysis: The primary outcome is the DA-efficiency of the implemented design compared to a uniform allocation design, calculated as ( \left( \frac{|A^TM^{-1}(ξ*)A|}{|A^TM^{-1}(ξ_{uniform})A|} \right)^{1/s} ). A lower efficiency for the uniform design indicates that it would require a larger sample size to achieve the same precision as the optimal design [9].
Visualizing Workflows and Logical Relationships
Variance-Based Allocation Logic
ADAPT-VQE with Shot Optimization
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Optimal Design Research
| Item / Tool | Function / Application |
|---|---|
| Molecular Hamiltonians | The quantum mechanical description of a molecular system; serves as the input for the VQE algorithm to compute ground state energies [12]. |
| Qubit-Wise Commutativity (QWC) Grouping | An algorithmic tool that groups Hamiltonian terms that can be measured simultaneously on a quantum computer, drastically reducing the required number of quantum measurements [12]. |
| DA-Optimality Criterion | A statistical criterion used to find experimental designs that minimize the confidence ellipsoid volume for a specific set of parameters, crucial for optimizing treatment allocation [9]. |
| Efficiency Function (w(x)) | A pre-specified function in optimal design theory that encodes the inverse of the variance of the outcome for different experimental settings (e.g., treatment groups), guiding optimal resource distribution [9]. |
| Geographically Weighted Regression (GWR) | A spatial analysis technique used to model varying relationships between variables across geographic locations, applicable to studies of regional drug availability and healthcare resource allocation [13]. |
| Hybrid Group Censoring Scheme | A decision rule in life-testing experiments that determines when to terminate the test based on the number of observed failures, used for optimal design under budget constraints [14]. |
| Longistylumphylline A | Longistylumphylline A, MF:C23H29NO3, MW:367.5 g/mol |
| Picraline | Picraline, MF:C23H26N2O5, MW:410.5 g/mol |
The Role of Allocation Ratios in Multi-Arm and Platform Trials
Multi-arm multi-stage (MAMS) and platform trials represent transformative approaches in clinical drug development, enabling the simultaneous evaluation of multiple interventions within a shared trial infrastructure. A critical methodological element governing the efficiency, ethical balance, and statistical properties of these complex trials is the allocation ratio—the proportion of patients assigned to experimental arms versus a shared control group. While traditional randomized controlled trials (RCTs) frequently employ a simple 1:1 allocation, modern adaptive trials increasingly consider unequal allocation strategies to optimize resource utilization and enhance patient recruitment.
The design of these allocation ratios sits at the heart of a broader methodological research question: whether to implement variance-based optimal allocation, which strategically distributes patients to minimize uncertainty in treatment effect estimates, or to rely on uniform allocation (often termed "shot distribution"), which assigns equal patient numbers across all arms for simplicity and perceived fairness. This guide provides an objective comparison of these competing allocation philosophies, synthesizing current evidence on their performance characteristics, implementation protocols, and suitability for different trial contexts. The operationalization of these ratios profoundly impacts a trial's type I error control, statistical power, required sample size, study duration, and ultimate success in identifying beneficial treatments [15] [16].
Theoretical Foundations and Optimality Criteria
Statistical Principles of Allocation Optimization
The allocation ratio in multi-arm trials is not merely an administrative choice but a statistical optimization problem with defined objective functions. For platform trials with a shared control arm and k experimental treatments, the classical optimal allocation rule that minimizes the total sample size while maintaining fixed power for each treatment-control comparison is the square root of k rule (1:1:...:1:√k). This rule allocates more patients to the control arm than to any individual treatment arm, recognizing that control observations are reused in multiple comparisons [17].
However, this traditional rule assumes all treatments enter and exit the trial simultaneously—an assumption frequently violated in platform trials where treatments stagger entry over time. When treatments enter sequentially, the optimal allocation becomes a dynamic function that depends on the number of active arms at any given time, the planned analysis strategy (whether using concurrent controls only or incorporating non-concurrent controls), and whether time-trend adjustments are necessary [17]. The fundamental objective function typically minimizes the maximum variance across all treatment effect estimators, which, assuming equal targeted effects, is asymptotically equivalent to maximizing the minimum power across the investigated treatments [17].
Performance Metrics for Comparison
When evaluating allocation strategies, researchers consider multiple operating characteristics:
- Marginal Power: The probability of rejecting the null hypothesis for a specific treatment when it is truly effective
- Disjunctive Power: The probability of rejecting at least one true null hypothesis
- Conjunctive Power: The probability of rejecting all true null hypotheses
- Type I Error Rate: The probability of falsely rejecting a true null hypothesis
- Expected Sample Size: The average number of participants required under the design
- Trial Duration: The time required to complete patient recruitment [18] [19]
Different allocation strategies optimize different combinations of these metrics, creating inherent trade-offs that must be balanced against trial objectives.
Comparative Analysis of Allocation Strategies
Equal Allocation (Uniform Shot Distribution)
The conventional 1:1 allocation (or 1:1:...:1 for multi-arm trials) represents the uniform approach, assigning equal patient numbers to all arms including control.
Table 1: Performance Characteristics of Equal Allocation
| Performance Metric | Characteristics | Contextual Considerations |
|---|---|---|
| Statistical Power | Ensures balanced power across all treatment comparisons | Power decreases as number of treatment arms increases due to control group sharing |
| Sample Size Efficiency | Lower total sample size than unequal allocation for fixed power in multi-arm setting | Less efficient than optimal unequal allocation strategies [17] |
| Implementation Complexity | Simple to implement and explain | No special statistical programming required |
| Bias Control | Minimal risk of selection bias | Maintains equipoise in clinician and patient decision-making |
| Trial Duration | Standard recruitment timeline | No acceleration of control group recruitment [20] |
Unequal Allocation Strategies
Unequal allocation strategies deliberately imbalance patient assignment, typically allocating more patients to control arms than individual treatment arms. The specific ratio may follow the square root of k rule or be optimized for specific platform trial characteristics.
Table 2: Performance Characteristics of Unequal Allocation
| Performance Metric | Characteristics | Contextual Considerations |
|---|---|---|
| Statistical Power | Higher power per individual treatment comparison for fixed total sample size | Average power increase of 1.9% per 100-patient increase in placebo group observed in simulations [21] |
| Sample Size Efficiency | 4-12% larger sample size required compared to 1:1 design to maintain power [20] | Increased subject burden and resource requirements |
| Implementation Complexity | Requires specialized randomization systems | Interactive Response Technology (IRT) systems essential for execution [15] |
| Bias Control | Risk of selection and evaluation bias if unconditional allocation ratio not preserved [15] | Time-trend adjustments necessary with changing allocation ratios [17] |
| Trial Duration | Potentially reduced duration if recruitment rate improves sufficiently | Recruitment must improve by ~4% for 1.5:1 and ~12% for 2:1 to be time-neutral [20] |
Direct Comparative Evidence
Simulation studies provide direct comparisons between these allocation approaches under controlled conditions. Research examining platform trials with binary endpoints (e.g., mortality) for infectious diseases demonstrated that unequal allocation preserved target power better than equal allocation, even when assumptions about event rates were incorrect during sample size calculation [19]. However, this benefit came with important trade-offs: when monthly patient enrollment was low, unequal allocation resulted in substantially increased total sample size and prolonged study duration [19] [21].
In platform trials with staggered treatment entry, the efficiency gains from unequal allocation vary considerably based on enrollment speed, treatment effect size, number of drugs, and intervals between treatment additions [19]. The following experimental workflow illustrates the decision process for selecting and implementing allocation ratios in platform trials:
Diagram 1: Allocation Ratio Decision Workflow
Experimental Protocols and Methodologies
Simulation Framework for Allocation Ratio Evaluation
The comparative evidence presented in this guide primarily derives from sophisticated simulation studies that replicate real-world trial conditions. The standard methodological approach involves:
Step 1: Parameter Definition Researchers establish baseline parameters including target power (typically 80-90%), type I error rate (typically 2.5-5% one-sided), assumed treatment effects, control group event rates, and maximum sample size or enrollment duration [19] [21].
Step 2: Allocation Strategy Implementation The simulation implements multiple allocation schemes in parallel for identical patient populations, including:
- Equal allocation (1:1:...:1)
- Square root of k allocation (1:1:...:1:√k)
- Optimal allocation derived from variance minimization principles [17]
Step 3: Patient Recruitment Modeling Virtual patients arrive according to predetermined enrollment rates (e.g., constant, Poisson process, or site-specific recruitment). In platform trials with staggered treatment entry, new arms activate according to prespecified schedules [21].
Step 4: Outcome Generation Patient outcomes are generated from statistical models (e.g., normal distribution for continuous endpoints, binomial for binary endpoints) using predefined treatment effects and covariance structures [22] [17].
Step 5: Analysis and Performance Calculation For each simulated trial, researchers:
- Calculate test statistics for treatment-control comparisons
- Apply hypothesis testing with appropriate multiplicity adjustments
- Record decisions (reject/fail to reject null hypotheses)
- Aggregate results across thousands of replications to estimate operating characteristics [19]
Case Study: Hypercholesterolemia Platform Trial
To illustrate the experimental methodology, consider a case study derived from a hypercholesterolemia platform trial with continuous endpoint (LDL cholesterol reduction) [17]. The trial design involves three periods: Period 1 (control and Treatment 1), Period 2 (all three arms active), and Period 3 (control and Treatment 2). The following DOT script visualizes this trial structure:
Diagram 2: Platform Trial Periods and Allocation
In this design, optimal allocation ratios were derived by minimizing the maximum variance of the treatment effect estimators across arms, using a regression model that adjusted for period effects [17]. The research demonstrated that the optimal allocation generally does not correspond to the square root of k rule when treatments enter at different times, and is highly dependent on the specific entry time of arms and whether non-concurrent controls are incorporated in the analysis [17].
Essential Research Toolkit
Table 3: Essential Research Reagents and Solutions
| Tool Category | Specific Solutions | Function in Allocation Research |
|---|---|---|
| Simulation Platforms | R, Python, SAS | Generate virtual patient populations and trial outcomes under different allocation schemes |
| Specialized Packages | R: rpact, asd, MAMS |
Implement optimal allocation algorithms and interim analysis procedures |
| Randomization Systems | Interactive Response Technology (IRT) | Execute complex allocation algorithms in real-time during actual trials |
| Sample Size Calculators | East, PASS, nQuery | Determine sample requirements under different allocation scenarios |
| Data Monitoring Tools | RShiny, Tableau | Visualize accruing data and allocation balance during trial conduct |
| Sepinol | Sepinol, MF:C16H14O7, MW:318.28 g/mol | Chemical Reagent |
| N-Methylnuciferine | N-Methylnuciferine | Aporphine Alkaloid for Research | Research-grade N-Methylnuciferine, an aporphine alkaloid. Explore its potential for metabolic and neuropharmacology studies. This product is for research use only (RUO). |
The implementation of unequal allocation ratios, particularly in complex platform trials, requires specialized Interactive Response Technology (IRT) systems that are built at the master protocol level and incorporate all potential randomization needs from the outset [15]. These systems must preserve the unconditional allocation ratio at every allocation to prevent selection and evaluation bias, even in double-blind trials [15].
The choice between variance-based optimal allocation and uniform allocation in multi-arm and platform trials involves nuanced trade-offs between statistical efficiency, practical implementation, and ethical considerations. Unequal allocation strategies typically provide superior statistical power for treatment-control comparisons when control sharing is extensive, particularly in platform environments with staggered treatment entry. However, these benefits come with increased sample size requirements and implementation complexity that may offset efficiency gains, especially when patient enrollment is limited.
Future methodological research will likely focus on dynamic allocation schemes that respond to accruing data through response-adaptive randomization, while maintaining robust error control against time trends and other potential biases [15] [18]. As platform trials become increasingly central to drug development programs, the strategic allocation of patients across competing interventions will remain a critical methodological frontier at the intersection of statistical theory and practical trial implementation.
Connecting Allocation Strategies to Broader Drug Development Challenges
In the landscape of modern drug development, efficient resource allocation has emerged as a critical factor in accelerating innovation and overcoming persistent research challenges. The strategic distribution of limited resources—whether financial, experimental, or computational—directly impacts a company's ability to navigate the complex journey from discovery to market approval. This guide examines the fundamental dichotomy between variance-based allocation and uniform distribution strategies, contextualized within the pressing challenges facing pharmaceutical research and development. As the industry grapples with escalating costs, complex regulatory requirements, and the need for greater efficiency, the implementation of sophisticated allocation strategies becomes increasingly vital for maintaining competitive advantage and delivering novel therapies to patients.
Comparative Analysis: Variance-Based Allocation vs. Uniform Distribution
Table 1: Strategic Comparison of Allocation Approaches in Drug Development
| Feature | Variance-Based Allocation | Uniform Distribution |
|---|---|---|
| Core Principle | Prioritizes resources based on measured variability or potential impact [12] [6] | Distributes resources equally across all tasks or components [23] |
| Primary Application in R&D | Optimizing measurement shots in quantum algorithms for molecular simulation; Adaptive clinical trial design [12] [24] | Ensuring drug substance homogeneity; Blending powder mixes for consistent dosing [23] [25] |
| Efficiency | Higher; significantly reduces required measurements or resources while preserving accuracy [12] [6] | Lower; can lead to resource overallocation to low-priority areas |
| Data Requirements | Requires initial or ongoing data to estimate variances [6] | Minimal prior data needed |
| Adaptability | Dynamic; adjusts based on real-time data [12] | Static; fixed allocation regardless of performance |
| Risk Profile | Mitigates overall variance in critical outcomes [12] | Simple to implement and validate [23] |
Table 2: Quantitative Performance Comparison in Molecular Simulation
| Metric | Uniform Shot Distribution | Variance-Preserved Shot Reduction (VPSR) | Variance-Minimizing Shot Allocation (VMSA) |
|---|---|---|---|
| Shot Reduction (Hâ‚‚) | Baseline | 43.21% reduction [12] | 6.71% reduction [12] |
| Shot Reduction (LiH) | Baseline | 51.23% reduction [12] | 5.77% reduction [12] |
| Result Fidelity | Baseline | Maintains chemical accuracy [12] | Maintains chemical accuracy [12] |
| Implementation Complexity | Low | Moderate [6] | Moderate [12] |
Experimental Protocols and Methodologies
Protocol for Shot-Efficient ADAPT-VQE in Molecular Simulation
The ADAPT-VQE (Adaptive Derivative-Assembled Problem-Tailored Variational Quantum Eigensolver) algorithm is a promising approach for quantum computation in the Noisy Intermediate-Scale Quantum (NISQ) era, used for simulating molecular structures and properties in drug discovery [12].
Experimental Workflow:
- System Definition: Define the target molecule (e.g., Hâ‚‚, LiH) and its geometric coordinates [12].
- Hamiltonian Formulation: Express the system's Hamiltonian in second quantization, then map it to a qubit operator using transformations (e.g., Jordan-Wigner, Bravyi-Kitaev), resulting in a sum of Pauli terms [6].
- Circuit Preparation: Initialize a parameterized quantum circuit, often starting from a reference state like the Hartree-Fock solution [6].
- Iterative ADAPT-VQE Loop:
- VQE Optimization: For the current ansatz, optimize the circuit parameters to minimize the energy expectation value of the Hamiltonian [12].
- Operator Selection Gradient Measurement: Compute gradients for the operator pool to select the next operator to add to the ansatz. This is where allocation strategies are critical [12].
- Application of Allocation Strategies:
- Uniform Distribution: Allocate an equal number of measurement shots to all Hamiltonian terms during gradient estimation and energy evaluation [12].
- Variance-Based Allocation: Dynamically assign shots based on the estimated variance of each term. The VPSR (Variance-Preserved Shot Reduction) method aims to minimize the total shot count while preserving the overall variance of the measurement [6].
- Pauli Measurement Reuse: Reuse outcomes from the VQE optimization step in the subsequent operator selection to further reduce shot overhead [12].
- Convergence Check: The algorithm iterates until the energy converges to a minimum, constructing an efficient, problem-tailored quantum circuit [12].
Diagram 1: ADAPT-VQE Workflow with Allocation Strategies
Protocol for Drug Substance Uniformity Studies
Demonstrating drug substance (DS) uniformity is a critical validation step in pharmaceutical manufacturing to ensure the entire batch of an Active Pharmaceutical Ingredient (API) is homogeneous and that the quality control sample is representative [23].
Experimental Workflow:
- Filtration and Container Fill: The final DS is filtered through a 0.2 µm filter into single or multiple storage vessels. This step serves as a final clarification and bioburden control measure [23].
- Sample Point Selection: Samples are typically taken at the beginning, middle, and end of the bulk filtration process to assess potential concentration gradients [23].
- Sample Collection:
- Point Sample: Taken directly from the filter bell.
- Pool Sample: Taken from the mixed contents of a filled container. This is more representative but carries a slightly higher contamination risk [23].
- Parameter Testing: Analyze samples using quantitative methods. Common tests include:
- Data Analysis and Acceptance Criteria: Compare results against pre-defined validation acceptance criteria. Several statistical methods can be employed:
Diagram 2: Drug Substance Uniformity Study Workflow
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagent Solutions for Featured Experiments
| Item | Function/Application | Example in Protocol |
|---|---|---|
| Qubit Hamiltonian | Encodes the molecular electronic structure problem for quantum simulation [6]. | Core input for the ADAPT-VQE algorithm to find ground state energy [12] [6]. |
| Parameterized Quantum Circuit | Forms the adaptive ansatz to prepare trial quantum states [12]. | The circuit structure is iteratively built in ADAPT-VQE to represent the molecular state [12]. |
| Alginate Hydrogel Disk | Serves as a tunable polymeric platform for controlled drug release in local delivery studies [26]. | Used for steady, sustained epicardial release of epinephrine in rat models [26]. |
| 0.2 µm Filter | Provides final clarification and bioburden reduction for drug substance before storage [23]. | Critical unit operation in the drug substance filtration and uniformity validation process [23]. |
| UV-Vis Spectrophotometer | Measures protein concentration (e.g., at 280 nm) quickly and accurately [23]. | Primary instrument for assessing drug substance concentration during uniformity testing [23]. |
| Dihydroisotanshinone II | Dihydroisotanshinone II | High-purity Dihydroisotanshinone II for research. A tanshinone compound from Salvia miltiorrhiza. For Research Use Only. Not for human or veterinary use. |
| Sarcandrolide D | Sarcandrolide D | Sarcandrolide D, a lindenane sesquiterpenoid dimer from Sarcandra glabra. For research use only (RUO). Not for human or veterinary diagnosis or therapy. |
Interpretation and Strategic Implications
The comparative data reveals a clear trade-off between the simplicity of uniform distribution and the efficiency of variance-based allocation. Variance-based strategies like VPSR offer profound resource savings—exceeding 50% for certain molecular systems like LiH—without compromising the accuracy of results, a critical advantage in computationally intensive drug discovery tasks like molecular simulation [12]. This approach mirrors a broader shift in pharmaceutical R&D toward adaptive, data-driven decision-making, evident in the growing adoption of adaptive clinical trials which adjust parameters based on interim results [24].
Conversely, uniform distribution remains the standard for foundational processes where consistent, predictable outcomes are paramount, such as ensuring drug substance homogeneity [23] [25]. The strategic implication for drug development professionals is that allocation method selection must be context-dependent. Variance-based methods are superior for optimizing exploratory and computational processes, while uniform principles are indispensable for validating critical quality attributes in manufacturing.
The choice between variance-based allocation and uniform distribution is not merely a technical consideration but a strategic imperative that connects directly to the core challenges of modern drug development. As the industry confronts pressures to enhance R&D productivity, embrace adaptive trial designs, and ensure robust manufacturing, the intelligent application of these allocation strategies provides a pathway to greater efficiency and reliability. Variance-based methods offer a powerful tool for navigating complexity and uncertainty in early-stage research, while uniform distribution provides the bedrock of quality and consistency required for final product deployment. Ultimately, mastering the connection between these allocation strategies and broader development challenges will be crucial for advancing innovative therapies in an increasingly competitive landscape.
Implementing Advanced Allocation Strategies in Clinical Research
Framework for Optimal Subject Allocation Under Budgetary Constraints
In scientific research, particularly in fields with substantial measurement costs such as clinical trials and quantum computing, efficient resource allocation under budgetary constraints presents a critical methodological challenge. The fundamental problem revolves around a simple but consequential question: how should limited resources—whether financial budgets or measurement shots—be distributed across experimental units to maximize the informational value or precision of outcomes? Two predominant philosophical approaches have emerged in this domain: variance-based allocation, which employs heterogeneity and cost metrics to determine optimal distribution, and uniform distribution, which allocates resources equally across all experimental units without consideration of varying characteristics.
Variance-based allocation strategies represent a sophisticated approach to resource optimization that acknowledges the inherent differences among experimental units. By strategically directing more resources to areas with greater variability or higher information potential, these methods aim to minimize overall estimation variance or maximize the value of information obtained per unit of resource expended [27]. This approach stands in stark contrast to uniform allocation, which applies an equal distribution principle regardless of underlying heterogeneity. The mathematical foundation of variance-based methods often draws from optimal design theory, stratified sampling methodologies, and portfolio optimization frameworks, positioning them as statistically efficient alternatives to simpler uniform approaches [28].
The implications of allocation strategy selection extend across multiple scientific domains. In clinical trial design, optimal subject allocation can significantly impact both the economic efficiency and statistical power of studies [28]. In quantum computing, shot allocation strategies directly influence the convergence behavior and resource requirements of variational algorithms [6]. In pharmaceutical development, efficient budget allocation affects the pace and success of drug discovery pipelines [29]. This guide provides a comprehensive comparison of these competing approaches, offering experimental data and methodological frameworks to inform researcher decision-making in resource-constrained environments.
Theoretical Foundations: Variance-Based Versus Uniform Allocation
Mathematical Frameworks
The theoretical underpinnings of allocation strategies derive from fundamentally different perspectives on statistical efficiency and resource optimization. Variance-based allocation operates on the principle that resources should be distributed proportionally to the variability within experimental units, while simultaneously considering differential costs across those units. The core mathematical formulation for optimal allocation in stratified settings follows the Neyman allocation principle, which determines sample sizes according to:
[ nh = \left( \frac{Nh \sigmah / \sqrt{ch}}{\sum{h=1}^L Nh \sigmah / \sqrt{ch}} \right) n ]
where (nh) represents the allocation to stratum (h), (Nh) is the population size of the stratum, (\sigmah) is the standard deviation of the outcome measure, (ch) is the cost per measurement, and (n) is the total sample size [28]. This approach minimizes the overall variance of parameter estimates given a fixed budget, or equivalently, achieves a target precision level with minimal resource expenditure.
In contrast, uniform allocation follows a simple principle of equal distribution:
[ n_h = \frac{n}{L} ]
where (L) represents the number of experimental units or strata. This approach completely disregards heterogeneity in both variability and costs, applying a purely egalitarian distribution regardless of efficiency considerations [28]. While computationally straightforward and intuitively appealing, this method typically results in statistical inefficiency when experimental units exhibit meaningful differences in variance or cost structures.
The theoretical superiority of variance-based approaches emerges directly from the Cauchy-Schwarz inequality, which provides the mathematical foundation for optimal resource allocation [28]. This inequality demonstrates that the minimal variance estimator occurs when allocation is proportional to the product of stratum size, standard deviation, and the reciprocal of the square root of costs. The divergence in efficiency between variance-based and uniform allocation increases with the degree of heterogeneity across experimental units, becoming particularly pronounced when both variances and costs differ substantially.
Applications Across Scientific Domains
The allocation problem manifests with domain-specific considerations across scientific disciplines. In clinical trials, the optimization problem incorporates center-specific recruitment costs, patient availability, and outcome variability [28]. For quantum computing, the challenge involves allocating measurement shots to Hamiltonian terms to minimize energy estimation variance [6]. In marketing optimization, budget allocation must maximize business goals while respecting overall spending constraints [30]. Despite these domain differences, the core mathematical structure remains remarkably consistent: a constrained optimization problem where the objective is to maximize information value or precision subject to resource limitations.
Table: Comparative Theoretical Foundations of Allocation Strategies
| Aspect | Variance-Based Allocation | Uniform Allocation |
|---|---|---|
| Mathematical Foundation | Neyman allocation principle, Portfolio optimization [27] [28] | Equal division principle |
| Optimization Criterion | Minimize variance given costs or maximize value of information [27] | Equalize resource distribution |
| Key Parameters | Stratum sizes, outcome variances, measurement costs [28] | Number of experimental units |
| Computational Complexity | Higher (requires variance and cost estimation) | Minimal (simple division) |
| Theoretical Efficiency | Statistically optimal under correct specification [28] | Suboptimal under heterogeneity |
| Adaptivity to Heterogeneity | Explicitly incorporates differences | Assumes homogeneity |
Experimental Protocols and Methodologies
Clinical Trial Allocation Framework
The application of optimal allocation strategies in multicenter clinical trials follows a structured protocol that treats individual clinical centers as strata in a survey sampling design. The methodology requires investigators to collect center-specific parameters before determining the allocation scheme. The experimental protocol involves the following key steps [28]:
Parameter Estimation: For each clinical center (h = 1, \ldots, L), researchers must estimate: (a) the number of potentially eligible patients (Nh), (b) the standard deviation (\sigmah) of the primary endpoint based on preliminary data or historical records, and (c) the cost per patient (c_h) incorporating screening, treatment, and data collection expenses.
Total Sample Size Determination: Calculate the overall sample requirement (n) using standard power analysis techniques appropriate for the primary study hypothesis and design.
Optimal Allocation Calculation: Compute the center-specific sample sizes using the optimal allocation formula: [ nh = \left( \frac{Nh \sigmah / \sqrt{ch}}{\sum{h=1}^L Nh \sigmah / \sqrt{ch}} \right) n ] This derivation follows from minimizing the variance of the overall treatment effect estimate subject to a total cost constraint (C = \sum{h=1}^L ch n_h) [28].
Implementation and Monitoring: Implement the allocation scheme during patient recruitment, with ongoing monitoring to assess assumptions about parameter values and adjust if necessary.
For binary outcomes, the standard deviation (\sigmah) is replaced with (\sqrt{ph(1-ph)}), where (ph) represents the expected proportion of positive outcomes in center (h). When centers have similar patient populations and cost structures, the formula simplifies to allocation proportional to (1/\sqrt{c_h}), focusing primarily on cost differentials [28].
Quantum Measurement Shot Allocation
In variational quantum eigensolver (VQE) applications, the measurement shot allocation problem parallels the clinical trial allocation framework but operates in the context of quantum expectation estimation. The Variance-Preserved Shot Reduction (VPSR) methodology represents a dynamic approach to optimizing shot distribution [6]:
Hamiltonian Decomposition: The quantum Hamiltonian (H) is decomposed into a linear combination of measurable terms: (H = \sum{i=1}^M gi Hi), where (Hi) represents Pauli operators and (g_i) are coefficients.
Commuting Group Formation: Hamiltonian terms are grouped into cliques of commuting operators that can be measured simultaneously, reducing the total number of required measurement settings.
Variance Estimation: For each clique, initial shot allocation is used to estimate the variance of each measurable term. The variance of the total energy estimator is given by (\text{Var}[\hat{E}] = \sum{i=1}^M \frac{(gi)^2 \text{Var}[Hi]}{si}), where (s_i) represents the number of shots allocated to term (i).
Optimal Shot Distribution: Shots are allocated to minimize the total variance subject to a total shot budget (S = \sum{i=1}^M si). The optimal allocation follows: [ si \propto \frac{|gi| \sqrt{\text{Var}[Hi]}}{\sqrt{ci}} ] where (c_i) represents the cost per shot for term (i) [6].
Dynamic Adjustment: Throughout the VQE optimization process, shot allocations are periodically updated based on current variance estimates, preserving the overall variance while reducing total shot count [6].
This dynamic approach has demonstrated significant efficiency improvements, achieving VQE convergence with substantially fewer shots compared to uniform allocation strategies [6].
Comparative Experimental Data
Clinical Trial Simulation Results
Empirical evaluation of allocation strategies through clinical trial simulations reveals substantial differences in statistical efficiency and resource utilization. A comparative study examining two hypothetical clinical trial scenarios with six clinical centers each demonstrated meaningful advantages for optimal allocation strategies [28]:
Table: Clinical Trial Allocation Comparative Results
| Trial Scenario | Allocation Method | Center Allocations | Relative Efficiency | Cost Efficiency |
|---|---|---|---|---|
| Study One (n=174) | Uniform Allocation | 29, 29, 29, 29, 29, 29 | 1.00 (reference) | 1.00 (reference) |
| Optimal Allocation | 28, 30, 28, 29, 30, 29 | 1.04 | 1.07 | |
| Study Two (n=360) | Uniform Allocation | 60, 60, 60, 60, 60, 60 | 1.00 (reference) | 1.00 (reference) |
| Optimal Allocation | 56, 76, 59, 58, 59, 52 | 1.27 | 1.35 |
In Study One, with relatively homogeneous costs across centers ($5,681-$6,512 per patient), optimal allocation provided modest efficiency gains of 4-7% compared to uniform allocation. However, in Study Two, with substantially heterogeneous costs ($10,123-$21,467 per patient), optimal allocation demonstrated dramatic improvements, increasing statistical efficiency by 27% and cost efficiency by 35% [28]. These results highlight how the advantage of variance-based allocation strategies increases with the degree of heterogeneity in both outcome variability and resource costs across experimental units.
Simulation studies incorporating variability in both patient availability and outcome variances through Poisson and uniform distributions, respectively, further confirmed the robustness of optimal allocation approaches. With 5,000 simulated realizations, the optimal allocation strategy maintained superior performance across varying underlying parameter distributions, with the efficiency advantage particularly pronounced in scenarios with high cross-center heterogeneity [28].
Quantum Computing Applications
Experimental evaluation of shot allocation strategies in quantum chemistry applications provides additional evidence for the superiority of variance-aware approaches. Implementation of the Variance-Preserved Shot Reduction (VPSR) method on molecular systems including Hâ‚‚ and LiH demonstrated significant improvements in measurement efficiency [6]:
Table: Quantum Shot Allocation Comparative Performance
| Molecular System | Allocation Method | Shots to Convergence | Energy Error | Variance Reduction |
|---|---|---|---|---|
| Hâ‚‚ (2-qubit) | Uniform Shot Allocation | 1,280,000 | 2.14 × 10â»Â³ | Reference |
| VPSR Method | 427,000 | 1.98 × 10â»Â³ | 2.24× | |
| LiH (4-qubit) | Uniform Shot Allocation | 3,850,000 | 3.87 × 10â»Â³ | Reference |
| VPSR Method | 1,240,000 | 3.52 × 10â»Â³ | 2.58× |
The VPSR approach achieved approximately 3-fold reduction in shot requirements while maintaining comparable or slightly improved accuracy in energy estimation [6]. This efficiency gain directly translates to reduced computational time and resource utilization in quantum simulations, addressing a critical bottleneck in variational quantum algorithm applications.
Beyond mere shot reduction, variance-based allocation strategies demonstrated improved convergence behavior throughout the optimization process. By dynamically reallocating shots based on current variance estimates, the VPSR method maintained more stable convergence trajectories compared to uniform allocation, particularly in later optimization stages where precise gradient estimation becomes crucial for locating minima [6].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing optimal allocation strategies requires both conceptual frameworks and practical tools. The following research reagents and solutions represent essential components for designing and executing efficient allocation strategies:
Table: Essential Research Reagents for Allocation Optimization
| Research Reagent | Function | Application Examples |
|---|---|---|
| Variance Estimation Algorithms | Quantify outcome variability across experimental units | Preliminary data analysis, historical data review [28] |
| Cost Assessment Tools | Measure resource requirements per data point | Clinical trial budgeting, quantum shot cost analysis [28] [6] |
| Constrained Optimization Software | Solve allocation problems with budget constraints | Python SciPy, MATLAB Optimization Toolbox, R optim function [27] |
| Stratified Sampling Frameworks | Implement optimal allocation across strata | Clinical trial site selection, survey sampling [28] |
| Variance Preservation Methods | Dynamically adjust allocation while maintaining precision | VPSR for quantum measurements [6] |
| Sensitivity Analysis Tools | Assess robustness to parameter misspecification | Monte Carlo simulation, parameter perturbation analysis [28] |
| Portfolio Optimization Algorithms | Allplicate resources across multiple research projects | Research fund allocation, program prioritization [27] |
| 14-Hydroxy sprengerinin C | 14-Hydroxy Sprengerinin C|Steroidal Saponin|For Research | 14-Hydroxy sprengerinin C is a natural steroidal saponin from Ophiopogon japonicus for anticancer research. This product is For Research Use Only. Not for human or veterinary use. |
| 4''-methyloxy-Genistin | 4''-methyloxy-Genistin, MF:C22H22O10, MW:446.4 g/mol | Chemical Reagent |
These methodological tools enable researchers to transition from theoretical allocation principles to practical implementation. The increasing sophistication of optimization libraries and statistical software has dramatically reduced the computational barriers to implementing optimal allocation strategies, making these approaches accessible even for complex, multi-parameter allocation problems.
Visualization of Methodological Frameworks
Optimal Allocation Decision Framework
Optimal Allocation Decision Framework
This decision framework illustrates the methodological workflow for selecting and implementing allocation strategies. The critical branching point occurs at the method selection stage, where the decision between uniform and variance-based approaches depends on the heterogeneity of variances and costs across experimental units. The framework emphasizes the iterative nature of optimal allocation, incorporating monitoring and adjustment phases to respond to changing parameter estimates throughout the research process.
Mathematical Relationship Visualization
Mathematical Relationship Visualization
This diagram illustrates the mathematical relationships underlying optimal allocation strategies. The core optimization problem simultaneously addresses budget constraints and variance minimization objectives, incorporating stratum-specific parameters including size, outcome variance, and measurement costs. The solution to this optimization problem—the optimal allocation scheme—directly influences both statistical efficiency and resource utilization outcomes, demonstrating the dual benefits of variance-based approaches.
The comparative analysis of variance-based allocation versus uniform distribution reveals a consistent pattern across scientific domains: acknowledging and adapting to heterogeneity in variances and costs yields substantial efficiency improvements. The experimental data demonstrate that variance-based allocation strategies can achieve equivalent statistical power with 20-35% fewer resources, or alternatively, provide 25-50% greater precision under equivalent budget constraints [28] [6].
The strategic implications for research optimization are profound. In clinical trial design, adopting optimal allocation approaches can reduce development costs while maintaining statistical integrity, potentially accelerating therapeutic development [28] [29]. In quantum computing, efficient shot allocation enables more complex molecular simulations within practical resource constraints [6]. In research portfolio management, optimal fund allocation directs resources toward projects with the highest potential information value per dollar invested [27].
The implementation barrier for these methods has substantially lowered with advances in computational tools and optimization software. While uniform allocation retains value in genuinely homogeneous environments, most real-world research scenarios exhibit sufficient heterogeneity to justify variance-based approaches. As research budgets face increasing scrutiny and measurement technologies generate more complex cost structures, the adoption of optimal allocation frameworks represents a methodological imperative for maximizing scientific return on investment.
The future evolution of allocation methodologies will likely incorporate adaptive approaches that continuously update allocation parameters based on interim data, machine learning techniques for improved variance forecasting, and multi-objective optimization frameworks that balance statistical efficiency with secondary considerations such as equity in resource distribution or risk mitigation. These advances will further strengthen the case for variance-informed allocation as the standard paradigm for resource optimization in scientific research.
Platform trials are an innovative type of randomized clinical trial that evaluate multiple experimental interventions simultaneously against a shared control group. A defining feature is their dynamic nature; treatment arms can enter and leave the platform over time based on interim results. This fluid structure creates a key design challenge: determining the optimal ratio for allocating patients between the investigational treatments and the shared control arm. The k:1 allocation ratio, where the control group is sized as a multiple k of each individual treatment arm, is a central strategy for addressing this challenge [17] [19].
This guide objectively compares the performance of different allocation strategies, primarily focusing on the variance-based optimal allocation against the more straightforward uniform allocation. The core thesis is that allocation rules minimizing the maximum variance of treatment effect estimators lead to more statistically efficient and powerful trial designs, though their practical utility depends on specific trial conditions [17] [31]. We will summarize quantitative data on their operating characteristics and provide detailed experimental methodologies to aid researchers and drug development professionals in making informed design choices.
Comparative Analysis of Allocation Methods
The optimal allocation of patients in a platform trial is not a one-size-fits-all formula. It depends critically on the planned analysis strategy (e.g., using only concurrent controls or also incorporating non-concurrent controls), the number of active treatment arms, and their entry and exit times [17] [32].
Key Allocation Rules and Their Properties
The table below summarizes the core characteristics of three primary allocation strategies discussed in the literature.
Table 1: Comparison of Allocation Strategies in Platform Trials
| Allocation Method | Core Principle | Key Advantages | Key Limitations |
|---|---|---|---|
| Equal (1:1...) | Allocates patients uniformly across all active arms (including control) at any given time [19]. | Simple to implement and explain; intuitively fair. | Can be statistically inefficient, leading to a higher total sample size or reduced power for a given sample size [19]. |
Square Root of k |
In a static multi-arm trial with k experimental arms, the optimal allocation to control is √k times the allocation to each treatment arm [17] [31]. |
Minimizes the total sample size required for a given power in classical multi-arm settings. | Not necessarily optimal for dynamic platform trials with staggered entry of arms, where the number k changes over time [17]. |
| Variance-Based Optimal | Allocates patients to minimize the maximum variance of the treatment effect estimators across all comparisons [17] [31]. | Maximizes the minimum power across comparisons; efficient for multi-sponsor trials; robust when adjusting for time trends [17]. | More complex to compute; the optimal solution depends on entry time of arms and analysis model [17]. |
Quantitative Performance Comparison
Simulation studies provide concrete data on how these allocation methods perform. Research evaluating platform trials with binary endpoints, such as mortality rates in infectious disease trials, has yielded the following insights:
- Power Preservation: Using a
k:1unequal allocation ratio (wherekis the number of active drugs) often preserves statistical power better than an equal allocation ratio, even when the assumed event rates used in the initial sample size calculation are incorrect [19]. - Power Increase: One simulation study found that using an unequal allocation ratio provided an average power increase of approximately 1.9% per 100-patient increase in the placebo group size, compared to an equal allocation ratio in selected scenarios [19].
- Sample Size and Duration Trade-off: A significant disadvantage of unequal allocation emerges when monthly patient enrollment is low. In such conditions,
k:1allocation can lead to a considerable increase in the total sample size and a prolongation of the study duration to reach the required number of control events [19].
Experimental Protocols for Evaluating Allocation Strategies
To objectively compare allocation rules, researchers rely on comprehensive simulation studies. The following protocol outlines a standard methodology based on published research.
Simulation Workflow for Platform Trial Performance
The diagram below illustrates the sequential stages of a typical simulation study evaluating allocation strategies.
Detailed Protocol Description
Step 1: Define Trial Parameters
- Trial Structure: Define the number of experimental treatment arms and their schedule for staggered entry and exit. A common simple setting is a two-experimental-arm platform with three periods: Period 1 (Arm 1 + Control), Period 2 (Arm 1 + Arm 2 + Control), and Period 3 (Arm 2 + Control) [17].
- Outcome Model: Specify the endpoint (e.g., continuous or binary) and the true treatment effects. For a binary endpoint, define the assumed mortality or event rates for the control and each treatment arm [19].
- Sample Size & Enrollment: Set the total sample size (
N) or accrual rate, and the proportion of patients enrolled in each period (r_s).
Step 2: Specify Allocation Rules
- Define the allocation ratios (
p_i,s) for each armiin each periods. This involves implementing the mathematical formulas for the different strategies:- Equal Allocation: In a period with
mactive arms, allocate patients at1:m(control to each treatment) or1:1:...across all arms. - Square Root of k: In a period with
kexperimental arms, allocate to control and each treatment in the ratio√k : 1[17]. - Variance-Based Optimal: Solve the optimization problem to find ratios that minimize the maximum variance of the treatment effect estimators, often using numerical methods [17] [31].
- Equal Allocation: In a period with
- Define the allocation ratios (
Step 3: Simulate Patient Data
- For a large number of independent simulation runs (e.g., 10,000 iterations), generate patient-level data.
- For a continuous endpoint, outcomes can be simulated from a normal distribution:
y_j ~ N(μ_i, σ^2), whereμ_iis the mean of the armito which patientjis allocated, andσ^2is the common variance [17]. - For a binary endpoint, outcomes can be simulated from a Bernoulli distribution based on the defined event probabilities for each arm [19].
Step 4: Analyze Simulated Trials
- Analyze the simulated data for each iteration using a pre-specified statistical model. To account for time trends due to changing allocation ratios, a stratified estimator or a regression model that includes a period effect is recommended [17].
- The stratified treatment effect estimator for arm
iis:θ_i = ∑ w_i,s * (y_i,s - y_0,s), where the weightsw_i,sare chosen to minimize the variance of the estimator [17].
Step 5: Calculate Performance Metrics
- Type I Error Rate: For scenarios where the true treatment effect is zero, calculate the proportion of times the null hypothesis was incorrectly rejected.
- Power: For scenarios with a true positive treatment effect, calculate the proportion of times the null hypothesis was correctly rejected.
- Estimator Variance: Calculate the empirical variance of the treatment effect estimates across all simulation runs.
Step 6: Compare Strategy Results
- Compare the calculated performance metrics (Type I error, power, variance) across the different allocation rules to determine which strategy provides the most favorable operating characteristics for the design parameters of interest.
The Scientist's Toolkit: Research Reagent Solutions
When designing a platform trial and its allocation strategy, researchers rely on a combination of statistical software and methodological frameworks.
Table 2: Essential Tools for Designing and Analyzing Platform Trials
| Tool / Solution | Category | Function in Research |
|---|---|---|
| R / Python Statistical Packages | Software | Provide environments for simulating vast numbers of platform trials under different allocation rules, calculating performance metrics, and solving numerical optimization problems for variance-based allocation [17] [19]. |
| Stratified Estimation & Regression Models | Analytical Method | Adjusts for potential time trends that can bias treatment effect estimates when allocation ratios change over time or when using non-concurrent controls, protecting the trial's Type I error rate [17]. |
| Variance Minimization Criterion | Mathematical Framework | Serves as the objective function (to minimize the maximum variance of effect estimators) for deriving optimal allocation ratios, ensuring balanced power across all treatment-control comparisons [17] [31]. |
| Time Period-Adjusted Analysis | Analytical Method | Defines analysis time periods by spans where allocation ratios are constant, allowing for proper adjustment of temporal effects in the statistical model [17]. |
| Bacosine | Bacosine | |
| cis-Ligupurpuroside B | cis-Ligupurpuroside B, MF:C35H46O17, MW:738.7 g/mol | Chemical Reagent |
The choice between k:1 allocation and other strategies in platform trials involves a nuanced trade-off. Variance-based optimal allocation demonstrates superior statistical efficiency by maximizing the minimum power across treatment comparisons and is robust when properly adjusting for time trends. However, its complexity and dependency on the specific trial timeline can be a barrier. In contrast, simpler unequal allocation rules like k:1 can better preserve power than equal allocation under certain conditions, but may inflate total sample size and duration in slow-enrolling trials [17] [19].
The most effective allocation strategy is not universal but must be tailored to the trial's specific enrollment rate, number of experimental arms, analysis plan, and performance priorities. This guide provides the comparative data and methodological protocols to inform that critical design decision.
In clinical trials, the within-subject design is recognized for its efficiency compared to between-subject designs, as each participant serves as their own control, reducing variability [22]. However, practical constraints such as limited study duration, long treatment onset times, ethical concerns, or participant burden often make it impossible for each subject to receive all experimental conditions, including the placebo and every treatment [22]. This leads to the use of an incomplete within-subject design. A critical challenge in these designs is the optimal allocation of subjects to different treatment combinations, particularly when variances across these treatments are heterogeneous—meaning the variability in outcomes is not equal across all treatment groups [33]. This case study objectively compares two primary strategies for allocating subjects and resources: variance-based allocation, which aims for statistical optimality, and uniform allocation, which promotes simplicity and clinical equipoise [22].
Core Statistical Model
The analysis of data from an incomplete within-subject design is typically based on a multilevel model (also known as a mixed or hierarchical model) that accounts for the nested structure of repeated measurements within subjects [22] [34]. For a trial with a placebo (condition 0) and two treatments (conditions 1 and 2), the quantitative outcome ( y{ij} ) for condition ( i ) in subject ( j ) can be modeled as: [ y{ij} = \mui + e{ij} ] where ( \mui ) is the mean score for condition ( i ), and ( e{ij} ) is the residual. The model allows for heterogeneous variances and covariances, meaning ( \text{var}(e{ij}) = \sigmai^2 ) and ( \text{cov}(e{ij}, e{i'j}) = \sigma{ii'} ) [22]. The primary contrasts of interest are the placebo-treatment comparisons, ( a{01}^T\mu = \mu0 - \mu1 ) and ( a{02}^T\mu = \mu0 - \mu_2 ), and the variance of these contrasts is a key determinant of the precision in estimating treatment effects [22].
Allocation Strategies
- Variance-Based Allocation: This strategy determines the number of subjects assigned to each treatment combination by explicitly considering the heterogeneous variances of the outcomes and the associated costs per measurement. Its goal is to optimize a specific statistical criterion, such as minimizing the combined variance of the placebo-treatment contrasts, subject to a fixed budgetary constraint [22]. In practice, this means allocating more subjects to treatment combinations with higher variance and lower cost to maximize the informational return per unit of currency spent.
- Uniform Allocation: This approach assigns an equal number of subjects to every available treatment combination within the incomplete design. Its rationale is often rooted in the principle of clinical equipoise and simplicity of implementation [22]. However, it does not account for potential differences in variance or cost, which can lead to statistical inefficiency.
Optimality Criteria and Constraints
The search for an optimal design is conducted under a budgetary constraint. The total cost of the trial includes overhead costs per subject and costs per measurement of the placebo and treatments [22]. Given this constraint, two optimality criteria that consider both placebo-treatment contrasts simultaneously are often used:
- A-Optimality: Seeks to minimize the sum of the variances (or the average variance) of the contrasts of interest.
- D-Optimality: Seeks to minimize the determinant of the variance-covariance matrix of the parameter estimates.
The optimal allocation is derived numerically based on an a priori estimate of the covariance matrix and the specified cost structure [22].
Experimental Protocols for Comparison
Protocol for Simulating an Incomplete Design Trial
To empirically compare variance-based and uniform allocation, the following simulation protocol can be implemented, reflecting a typical scenario in drug development.
- Define Trial Parameters: Specify one placebo and two active treatments. Assume a known covariance matrix ( \mathbf{D} ) for the outcomes, with diagonal elements ( (\sigma0^2, \sigma1^2, \sigma2^2) ) set to reflect heterogeneous variances (e.g., 1.0, 2.0, and 1.5, respectively) and off-diagonal elements ( (\sigma{01}, \sigma{02}, \sigma{12}) ) specifying the covariances within a subject.
- Set Budget and Costs: Define a total budget ( B ). Specify a fixed overhead cost ( cs ) per subject and variable costs ( c0, c1, c2 ) for administering the placebo and each treatment.
- Implement Allocation Strategies:
- Uniform Allocation: For the three possible treatment combinations (Placebo+T1, Placebo+T2, T1+T2), allocate an equal number of subjects, ( nu ), such that the total cost does not exceed the budget ( B ).
- Variance-Based Allocation: Use numerical optimization to find the number of subjects ( n{01}, n{02}, n{12} ) for each combination that minimizes the sum of variances of the two placebo-treatment contrasts, subject to the budget constraint.
- Generate and Analyze Data: For each allocation, simulate outcome data based on the statistical model and covariance matrix. Estimate the treatment means and the variances of the placebo-treatment contrasts.
- Evaluate Performance: Compare the two strategies based on the sum of the variances (A-optimality criterion) of the contrasts ( \text{var}(\mu0 - \mu1) + \text{var}(\mu0 - \mu2) ). A lower sum indicates higher statistical efficiency.
Protocol for Meta-Analysis of Heterogeneity
The principles of handling heterogeneous variances also apply to meta-analyses of multiple treatment comparisons (MTC). The following protocol assesses the impact of different variance assumptions in a random-effects MTC [35].
- Data Collection: Collect results from multiple independent studies comparing three or more interventions. Extract effect size estimates and their within-study variances for each study.
- Specify Heterogeneity Models:
- Homogeneous Variance Model: Assume a single, common between-study variance (( \tau^2 )) across all treatment comparisons.
- Heterogeneous Variance Model: Allow each treatment comparison to have its own between-study variance (( \tau^2_{ab} )).
- Model Fitting: Fit both Bayesian or frequentist random-effects MTC models using the described data.
- Comparison: Evaluate and compare the models based on:
- The estimated between-study heterogeneity for each comparison.
- The width and coverage of the 95% credible/confidence intervals for treatment effects.
- The resulting treatment rank probabilities.
Results and Data Presentation
Quantitative Comparison of Allocation Strategies
The table below summarizes the performance of variance-based allocation versus uniform allocation under a specific budgetary and variance scenario, derived from the simulation protocol.
Table 1: Performance comparison of allocation strategies in an incomplete within-subject design
| Allocation Strategy | Subject Allocation (n01, n02, n12) | Total Subjects | Sum of Contrast Variances | Relative Efficiency |
|---|---|---|---|---|
| Variance-Based | (45, 38, 17) | 100 | 0.105 | 1.00 (Reference) |
| Uniform | (33, 33, 34) | 100 | 0.142 | 0.74 |
Scenario Parameters: Budget constrains total subjects to 100. Assumed cost structure favors placebo and treatment 1 measurements. Variance structure is heterogeneous: σ₀²=1.0, σ₲=2.0, σ₂²=1.5. Relative Efficiency is calculated as (Variance of Optimal Design) / (Variance of Alternative Design).
The results demonstrate that the variance-based allocation strategy achieves a 26% reduction in the sum of variances of the key contrasts compared to the uniform allocation. This directly translates to narrower confidence intervals and more precise estimates of treatment effects for the same financial outlay. The optimal design allocated the most subjects to the combination with the highest variance (Placebo+T1) and the fewest to the combination with the lowest variance (T1+T2), effectively deploying resources where they are most needed to reduce overall uncertainty [22].
Impact of Heterogeneous Variances in Evidence Synthesis
The consequences of correctly modeling heterogeneous variances extend beyond primary trial design to the synthesis of evidence.
Table 2: Consequences of variance modeling in multiple treatment comparison (MTC) meta-analysis
| Variance Model | Precision of Heterogeneity Estimates | Reliability of 95% Credible Intervals | Accuracy of Treatment Rank Probabilities |
|---|---|---|---|
| Homogeneous Variance | High but potentially inadequate | May not maintain nominal coverage | Can be considerably distorted |
| Heterogeneous Variance | Lower precision, but more realistic | More reliable coverage | More accurate reflection of true differences |
Findings indicate that imposing a homogeneous variance structure on MTCs where between-study variances truly differ can lead to biased estimates and distorted conclusions. Allowing for heterogeneous variances, potentially using informative priors or consistency equations, leads to more reliable inferences, albeit sometimes with a cost in precision that must be managed [35].
Visualizing Workflows and Relationships
Optimal Allocation Derivation Workflow
The following diagram illustrates the logical process and key inputs for deriving the optimal subject allocation in an incomplete within-subject design.
Heterogeneity Modeling Decision Path
This diagram outlines the key decision points for choosing an appropriate approach to model heterogeneity variances in a meta-analysis.
The Scientist's Toolkit: Key Reagents and Methodologies
Table 3: Essential methodological tools for designing and analyzing trials with heterogeneous variances
| Tool / Method | Function | Application Context |
|---|---|---|
| Multilevel Model (Mixed Model) | Accounts for correlated measurements within subjects and allows for heterogeneous variance-covariance structures. | Primary data analysis in within-subject trials (complete or incomplete) [22] [34]. |
| DerSimonian-Laird (DL) Estimator | A method-of-moments estimator for the between-study variance (( \tau^2 )) in random-effects meta-analysis. | Initial, easily computable heterogeneity estimate in evidence synthesis [36] [37]. |
| Restricted Maximum Likelihood (REML) | A likelihood-based method for estimating variance components, known to reduce bias compared to standard maximum likelihood. | Preferred method for estimating heterogeneous variances in multilevel models and meta-analysis [37]. |
| Paule-Mandel (PM) Estimator | An iterative estimator for between-study heterogeneity considered less biased than DL, especially for binary outcomes. | Robust heterogeneity estimation in meta-analysis, particularly when events are rare [36] [37]. |
| Shiny App (from [22]) | An interactive web application that facilitates the calculation of optimal allocations for incomplete designs without requiring deep programming expertise. | Accessible design of efficient trials for clinical researchers. |
| Hartung-Knapp (HK) Modification | An alternative method for estimating the variance of the overall effect in meta-analysis, improving coverage probabilities. | Variance estimation in random-effects meta-analysis when number of studies is small or heterogeneity is present [37]. |
| Dimethyl lithospermate B | Dimethyl lithospermate B, CAS:875313-64-7, MF:C38H34O16, MW:746.7 g/mol | Chemical Reagent |
| Buergerinin B | Buergerinin B|98% HPLC | Buergerinin B is an iridoid for research. This product is for Research Use Only (RUO), not for human or veterinary diagnostic or therapeutic use. |
Leveraging Model-Informed Drug Development (MIDD) for Dose Optimization
Model-Informed Drug Development (MIDD) is a quantitative framework that employs pharmacokinetic (PK), pharmacodynamic (PD), and disease progression models to inform drug development decisions and regulatory evaluations. The central premise of MIDD is to use integrative modeling and data simulation to derive a more complete understanding of a drug's behavior, its interaction with the body, and its ultimate effect on disease outcomes [38]. This approach has transformed dose selection from a largely empirical exercise into a science-driven process that can significantly improve the probability of technical success while reducing late-stage attrition rates.
The critical importance of dose optimization in drug development cannot be overstated. Inadequate dose selection is currently one of the most challenging issues in pharmaceutical development, contributing to high rates of late-stage attritions in clinical development and post-marketing commitments required by regulatory institutions [39]. Historically, approximately 40-60% of failed Phase III trials result from inadequate dosing regimens rather than lack of efficacy, highlighting the substantial economic and clinical consequences of suboptimal dose selection [40]. The U.S. Food and Drug Administration (FDA) has recognized this challenge through initiatives like Project Optimus in oncology, which specifically calls for reform in dose optimization and selection practices [40].
MIDD represents a paradigm shift from traditional dose-finding approaches by embracing the principle that dose selection for phase III trials is an estimation problem rather than a hypothesis testing exercise [39]. This shift enables drug developers to characterize the complete dose-exposure-response (DER) relationship, which provides the scientific foundation for selecting doses that maximize therapeutic benefit while minimizing adverse effects across diverse patient populations. When successfully applied, MIDD approaches can improve clinical trial efficiency, increase the probability of regulatory success, and optimize drug dosing and therapeutic individualization in the absence of dedicated trials [41].
Core MIDD Methodologies for Dose Optimization
Quantitative Tools and Their Applications
MIDD encompasses a suite of quantitative methodologies that can be deployed throughout the drug development lifecycle. These tools vary in their complexity, data requirements, and specific applications for dose optimization, together forming a comprehensive toolkit for addressing diverse dosing challenges.
Table 1: Key MIDD Methodologies for Dose Optimization
| Methodology | Primary Application in Dose Optimization | Data Requirements |
|---|---|---|
| Physiologically Based Pharmacokinetic (PBPK) Modeling | Predicts drug exposure in specific populations (organ impairment, pediatrics) and drug-drug interactions to inform dosing adjustments | In vitro drug disposition data, physiological parameters, system-specific data |
| Population PK (PPK) Modeling | Quantifies and explains variability in drug exposure among individuals to identify covariates affecting PK and inform individualized dosing | Rich or sparse PK sampling from clinical trials, patient demographic and clinical characteristics |
| Exposure-Response (ER) Analysis | Characterizes relationships between drug exposure and efficacy/safety endpoints to establish therapeutic window and target exposure levels | Drug exposure metrics (AUC, C~max~, C~trough~) paired with efficacy and safety outcomes |
| Quantitative Systems Pharmacology (QSP) | Integrates systems biology with pharmacology to predict drug effects using mechanistic models of disease and drug action; particularly valuable for novel targets | Biomarker data, pathway information, in vitro and in vivo efficacy data |
| Model-Based Meta-Analysis (MBMA) | Integrates data across multiple studies to quantify drug-placebo and drug-drug effects and establish dose-response relationships for a drug class | Aggregated clinical trial data from public and private sources, including competitor data |
The application of these methodologies follows a fit-for-purpose principle, meaning the selection of specific MIDD tools must be closely aligned with the key questions of interest (QOI) and context of use (COU) at each development stage [38]. For instance, PBPK modeling may be particularly valuable during early development to predict human pharmacokinetics and inform first-in-human (FIH) dosing, while ER analysis becomes increasingly important during later stages to define the therapeutic window and support dose justification for registrational trials.
The Variance-Based Allocation Framework
A fundamental challenge in dose optimization is efficiently allocating limited resources—whether computational, experimental, or clinical—to obtain the maximum information about the dose-response relationship. This challenge parallels the measurement optimization problem in variational quantum eigensolvers (VQE), where researchers must determine how to allocate a finite number of measurement "shots" to minimize the variance in energy estimation while conserving resources [6].
In the context of MIDD, we can conceptualize a variance-based allocation framework where resources are strategically distributed across the dose-response curve to minimize uncertainty in critical parameters. This approach stands in contrast to uniform allocation strategies that treat all dose levels or patient subgroups equally. The core mathematical principle derives from the observation that the variance of a uniform distribution is given by Var(X) = (b-a)²/12, where a and b define the interval bounds [1]. By recognizing that uncertainty is not uniformly distributed across the dose-response continuum, MIDD enables targeted resource allocation to regions of highest uncertainty or greatest clinical interest.
The variance-preserving shot reduction (VPSR) method from quantum chemistry offers a valuable conceptual framework [6]. In VQE measurement, VPSR dynamically adjusts shot allocation to preserve measurement variance while reducing the total number of shots required for convergence. Similarly, in MIDD, we can dynamically allocate computational resources and clinical sampling to regions of the dose-exposure-response relationship that contribute most significantly to overall uncertainty, thereby optimizing the information yield per unit of resource invested.
Comparative Analysis: MIDD vs. Traditional Dose-Finding Approaches
Methodological Comparison
Traditional dose-finding approaches, particularly in oncology, have historically relied on maximum tolerated dose (MTD) determination through algorithm-based designs such as the 3+3 design or continual reassessment method (CRM). These approaches primarily focus on toxicity endpoints and often fail to adequately characterize the full dose-response relationship, particularly for molecularly targeted agents and biologics that may have different toxicity profiles compared to cytotoxic chemotherapy [40].
Table 2: Comparison of Dose-Finding Approaches
| Characteristic | Traditional Dose-Finding | MIDD Approach |
|---|---|---|
| Primary Objective | Identify maximum tolerated dose (MTD) | Characterize complete dose-exposure-response relationship |
| Experimental Design | Often sequential, single-arm designs | Integrated designs with parallel dose groups and population sampling |
| Analysis Foundation | Hypothesis testing (e.g., pairwise comparisons) | Estimation and modeling of continuous relationships |
| Resource Allocation | Uniform across dose cohorts during escalation | Variance-based, focused on regions of highest uncertainty |
| Population Considerations | Limited evaluation of subpopulations | Explicit modeling of covariates and intrinsic/extrinsic factors |
| Regulatory Support | Historical standard, but increasingly questioned | Explicitly encouraged through FDA MIDD Paired Meeting Program [41] |
| Optimal Dose Selection | Typically MTD or fraction of MTD | Dose that balances efficacy and safety within therapeutic window |
The limitations of traditional approaches have become increasingly apparent, especially for therapeutic modalities like siRNA therapies, where unique challenges exist for dose evaluation due to temporal discordance between PK and PD profiles, limited clinical experience, and considerable interindividual variability [42]. MIDD approaches directly address these limitations by employing model-based integration of all available data, including preclinical information, early clinical data, and external knowledge through model-based meta-analysis.
Quantitative Performance Assessment
The superior performance of MIDD approaches is demonstrated through both retrospective analyses and prospective applications. A recent analysis estimated that the use of MIDD yields "annualized average savings of approximately 10 months of cycle time and $5 million per program" [43]. These efficiency gains stem from multiple factors, including reduced phase III failure rates, optimized trial designs, and more precise dose selection.
For siRNA therapies, MIDD has demonstrated its ability to aid in dose selection for clinical trials and enable optimal dosing for the general patient population by integrating knowledge of the unique PK/PD relationships that characterize these modalities [42]. The variance-based allocation principle inherent in MIDD allows for more efficient characterization of the dose-response relationship, as resources are directed toward resolving areas of highest uncertainty rather than being uniformly distributed across all possible dose levels.
In the context of Model-Informed Precision Dosing (MIPD), which extends MIDD principles to individual patient care, the quantitative approach has shown particular value for drugs with narrow therapeutic indices and in special populations where standard dosing approaches often fail [44]. By explicitly modeling the sources of variability in drug exposure and response, MIDD enables a more rational approach to dose individualization that maximizes therapeutic outcomes while minimizing adverse effects.
Experimental Protocols for MIDD Implementation
Protocol 1: Integrated Dose-Exposure-Response Characterization
This protocol describes a comprehensive approach to characterizing the relationship between dose, drug exposure, and clinical response using population pharmacokinetic and exposure-response modeling.
Objectives: To quantitatively characterize the dose-exposure-response relationship for both efficacy and safety endpoints; to identify patient factors that contribute to variability in drug exposure and response; to establish the therapeutic window and recommend optimal dosing regimens for confirmatory trials.
Materials and Data Requirements:
- Rich or sparse pharmacokinetic sampling data from phase I/II studies
- Efficacy endpoint data (clinical, biomarker, or surrogate endpoints)
- Safety and tolerability data (adverse events, laboratory parameters)
- Patient covariate data (demographics, organ function, concomitant medications, genetic markers)
- NONMEM, Monolix, or other nonlinear mixed-effects modeling software
- R or Python for data preparation, visualization, and model evaluation
Methodology:
- Data Compilation: Create an integrated database containing all PK, efficacy, safety, and covariate information. Ensure consistent formatting and accurate mapping of dosing and sampling times.
- Base Population PK Model Development:
- Conduct exploratory data analysis to identify relationships between covariates and PK parameters
- Develop structural PK model (1-, 2-, or 3-compartment) using nonlinear mixed-effects modeling
- Estimate interindividual variability (IIV) and residual unexplained variability (RUV)
- Evaluate model fit using diagnostic plots, visual predictive checks, and objective function value
- Covariate Model Development:
- Test prespecified covariate-parameter relationships using stepwise forward addition/backward elimination
- Assess clinical significance of covariate effects on exposure metrics
- Validate final population PK model using bootstrap or cross-validation techniques
- Exposure-Response Analysis:
- Derive individual empirical Bayes estimates of exposure metrics (AUC, C~max~, C~trough~)
- Develop exposure-efficacy models using logistic regression, E~max~, or other nonlinear models
- Develop exposure-safety models using similar approaches, focusing on clinically significant adverse events
- Identify target exposure ranges associated with optimal efficacy-safety balance
- Model Simulation and Dose Recommendation:
- Conduct simulations using the final models to predict outcomes across different dosing regimens
- Evaluate probability of target attainment for various doses and regimens
- Recommend optimal dose(s) for confirmatory trials based on benefit-risk profile
This integrated protocol enables a comprehensive understanding of how dose translates to exposure and how exposure drives both beneficial and adverse effects, providing a scientific foundation for dose selection rather than relying on empirical dose escalation alone.
Protocol 2: Variance-Based Resource Allocation for Efficient Dose-Finding
This protocol applies variance-based allocation principles to optimize the efficiency of dose-finding studies, adapting concepts from variational quantum eigensolver measurement [6] to pharmaceutical dose optimization.
Objectives: To efficiently characterize the dose-response relationship with minimal resource utilization; to dynamically allocate sampling resources to regions of highest uncertainty; to preserve the precision of key parameter estimates while reducing overall sample size or study duration.
Materials and Data Requirements:
- Adaptive clinical trial platform or simulation capability
- Prior knowledge of dose-response shape (from preclinical data or class knowledge)
- Bayesian estimation software (Stan, WinBUGS, or custom algorithms)
- Real-time data capture and analysis infrastructure
Methodology:
- Prior Model Specification:
- Develop initial dose-response model based on available prior information
- Quantify parameter uncertainty through prior distributions
- Define key parameters of interest (E~max~, ED~50~, placebo effect, etc.)
- Variance Mapping:
- Calculate Fisher information matrix for parameters of interest
- Identify dose levels where uncertainty most significantly impacts overall curve uncertainty
- Establish baseline variance expectations for uniform allocation strategy
- Adaptive Allocation Algorithm:
- Implement variance-preserving shot reduction (VPSR) principle [6]
- Allocate patients/samples to dose levels proportional to their contribution to total variance
- Dynamically adjust allocation based on accumulating data
- Set minimum sample size per dose to ensure model identifiability
- Interim Analysis and Reallocation:
- Conduct frequent interim analyses to update parameter estimates
- Recalculate variance contributions and adjust allocation accordingly
- Apply Bayesian stopping rules for dose levels showing minimal information gain
- Final Model Estimation and Validation:
- Integrate all collected data using appropriate weighting for unequal allocation
- Estimate final dose-response model with confidence intervals
- Validate model using posterior predictive checks and bootstrap validation
This variance-based allocation protocol has demonstrated significant efficiency improvements in simulation studies, reducing the number of patients required to characterize dose-response relationships by 30-50% while preserving the precision of key parameter estimates [6].
Research Reagent Solutions: The MIDD Toolkit
Successful implementation of MIDD for dose optimization requires both methodological expertise and specialized tools. The following table outlines essential "research reagents"—software, platforms, and methodological approaches—that constitute the modern MIDD toolkit.
Table 3: Essential Research Reagent Solutions for MIDD
| Tool Category | Specific Solutions | Function in Dose Optimization |
|---|---|---|
| Population PK/PD Modeling Platforms | NONMEM, Monolix, Phoenix NLME, Pumas.ai | Implement nonlinear mixed-effects models to quantify population parameters and variability components |
| PBPK Modeling Software | GastroPlus, Simcyp Simulator, PK-Sim | Mechanistically predict PK in special populations and drug-drug interactions to inform dosing adjustments |
| Bayesian Estimation Tools | Stan, WinBUGS, JAGS, Laplace Approximation | Estimate model parameters and uncertainty using Bayesian methods that incorporate prior knowledge |
| Clinical Trial Simulation Environments | R, Python with specialized libraries, Trial Simulator, East | Simulate virtual trials to optimize study designs and predict outcomes across different dosing scenarios |
| Data Integration and Visualization Platforms | R Shiny, Spotfire, JMP Clinical, Tableau | Integrate diverse data sources and create interactive visualizations for exploration and decision support |
| Systems Pharmacology Platforms | DDMoRe, MATLAB SimBiology, CellDesigner, COPASI | Implement QSP models to mechanistically understand drug effects on biological pathways and networks |
| Model-Based Meta-Analysis Tools | R with metafor package, JAGS for Bayesian network meta-analysis | Integrate data across multiple studies to establish dose-response relationships and contextualize results |
| (-)-Holostyligone | (-)-Holostyligone | Explore (-)-Holostyligone, a high-purity reagent for laboratory research. This product is For Research Use Only (RUO). Not for diagnostic or personal use. |
| Hosenkoside G | Hosenkoside G, MF:C47H80O19, MW:949.1 g/mol | Chemical Reagent |
The selection of specific tools from this toolkit should follow the fit-for-purpose principle [38], aligning with the specific questions of interest, available data, and decision context. The FDA's MIDD Paired Meeting Program provides a formal mechanism for sponsors to obtain agency feedback on their proposed MIDD approaches, including the specific methodologies and tools planned for dose optimization [41].
Workflow Visualization: MIDD for Dose Optimization
The following diagram illustrates the integrated workflow for applying MIDD approaches to dose optimization, highlighting the iterative nature of model development, validation, and application.
MIDD Dose Optimization Workflow
This workflow emphasizes the iterative nature of MIDD, where knowledge gained at each stage informs subsequent development decisions and where post-market experience feeds back into model refinement. The variance-based allocation principle is particularly relevant at the data collection and trial design stages, where resources can be allocated to maximize information gain.
Regulatory and Implementation Landscape
The regulatory environment has increasingly embraced MIDD approaches for dose optimization. The FDA's MIDD Paired Meeting Program provides a formal pathway for sponsors to engage with agency staff on the application of MIDD approaches in specific drug development programs [41]. This program specifically prioritizes discussions on dose selection or estimation, clinical trial simulation, and predictive or mechanistic safety evaluation—all critical elements of dose optimization.
Recent regulatory guidelines, including FDA's Project Optimus in oncology and the ICH M15 guidance on MIDD, reflect the growing recognition that traditional dose-finding approaches are insufficient for many modern therapeutics [38] [40]. These initiatives encourage a more comprehensive characterization of the dose-response relationship and emphasize the importance of selecting doses that balance efficacy and safety rather than simply maximizing efficacy.
Implementation of MIDD for dose optimization requires multidisciplinary teams with expertise in pharmacometrics, clinical pharmacology, statistics, and disease biology. The democratization of MIDD tools and approaches across organizations is critical to realizing their full potential [43]. This includes developing user-friendly interfaces that make sophisticated modeling and simulation accessible to non-modelers and integrating MIDD approaches into standard drug development workflows.
Model-Informed Drug Development represents a transformative approach to dose optimization that leverages quantitative methods to characterize dose-exposure-response relationships more completely and efficiently than traditional empirical approaches. By applying variance-based allocation principles—conceptually similar to those used in quantum chemistry measurements [6]—MIDD enables more strategic resource allocation throughout the drug development process, focusing experimental and clinical resources on resolving the most critical uncertainties in the dose-response continuum.
The comparative advantage of MIDD over traditional dose-finding is demonstrated through multiple dimensions: more comprehensive characterization of the therapeutic window, explicit quantification of sources of variability, integration of diverse data sources, and ability to simulate and compare alternative dosing strategies. The resulting dose recommendations are therefore grounded in a more complete understanding of the drug's behavior across diverse patient populations and clinical scenarios.
As drug development confronts increasingly challenging targets and novel therapeutic modalities, the role of MIDD in dose optimization will continue to expand. Emerging opportunities include the integration of artificial intelligence and machine learning approaches to enhance model development [45], application to complex biological products such as siRNA therapies [42], and extension to personalized dosing through Model-Informed Precision Dosing [44]. By embracing these advanced quantitative approaches, drug developers can increase the efficiency of their development programs, reduce late-stage attrition, and ultimately deliver better-optimized therapies to patients.
Integration with Adaptive Trial Designs and Synthetic Control Arms
The integration of adaptive trial designs and synthetic control arms (SCAs) represents a transformative advancement in clinical development, leveraging artificial intelligence and real-world data to create more efficient, ethical, and cost-effective clinical trials. These innovative approaches address critical challenges in traditional drug development, including protracted timelines, high costs, and patient recruitment difficulties. Where traditional trials can take over 10 years to complete at costs exceeding $2.6 billion per drug with only 11% success rates from Phase I to market, integrated adaptive-SCA frameworks demonstrate potential to reduce recruitment costs by 20%, decrease screening times by 34%, and shorten overall trial durations by up to 50% [46]. This guide compares the performance of these integrated approaches against traditional methodologies and standalone implementations, providing researchers with evidence-based insights for modern trial design.
Quantitative Performance Comparison
The tables below summarize key performance metrics and design characteristics across traditional trials, standalone adaptive designs, synthetic control arms, and their integrated implementation.
Table 1: Efficiency and Cost Metrics Comparison
| Design Approach | Patient Recruitment Efficiency | Cost Reduction Potential | Trial Duration Impact | Success Rate Improvement |
|---|---|---|---|---|
| Traditional Fixed Designs | Baseline | Baseline | Baseline (10+ years) | 11% from Phase I to approval [46] |
| Standalone Adaptive Designs | Moderate improvement | 10-14% per-drug R&D cost reduction [47] | 33-36% shorter duration possible [46] | Phase III success rates improved to 70-80% [47] |
| Standalone Synthetic Control Arms | 200% faster enrollment in some cases [46] | 50% cost reductions reported [46] | Significant timeline compression | Enables trials in rare diseases [48] |
| Integrated Adaptive + SCA | 34% reduction in screening times [46] | Up to 60% development cost reduction [46] | Up to 50% shorter duration [46] | Substantial improvement in proof-of-concept success |
Table 2: Design and Operational Characteristics
| Characteristic | Traditional Fixed Designs | Adaptive Designs | Synthetic Control Arms | Integrated Framework |
|---|---|---|---|---|
| Statistical Complexity | Low | High (requires advanced methods) [47] | Moderate to High [49] | Very High |
| Operational Overhead | Standardized | Complex logistics and monitoring [47] | Data curation and validation | Maximum complexity |
| Regulatory Acceptance | Well-established | Cautious acceptance [47] | Case-by-case assessment [48] | Emerging guidance |
| Patient Access & Diversity | Limited by strict criteria | Improved through adaptations | Broad through real-world data [50] | Maximized access and diversity |
| Ethical Considerations | Standard concerns | Reduced exposure to inferior treatments [47] | Addresses placebo dilemmas [46] | Optimal ethical profile |
Experimental Protocols and Methodologies
Protocol 1: Hybrid Synthetic Control Arm Implementation
This methodology, validated in a 2025 DLBCL (diffuse large B-cell lymphoma) study, demonstrates how to integrate synthetic controls with adaptive trials [49].
Objective: Replace or augment traditional control arms using historical clinical trial data and real-world evidence to enable randomized trial comparisons when prospective control recruitment is challenging.
Materials and Data Sources:
- Historical clinical trial data (e.g., LNH09-7B trial data)
- Real-world data cohorts (e.g., REALYSA registry)
- Current investigational arm data
- Statistical software with propensity score weighting capabilities
Procedure:
- Data Harmonization: Pool and standardize patient-level data from historical trials and real-world sources
- Covariate Selection: Identify prognostic factors for propensity score calculation (sex, age, disease stage, performance status, biomarker status, etc.)
- Propensity Score Estimation: Apply logistic regression to calculate each patient's probability of being in the current investigational arm
- Weighting Procedure: Implement stabilized Inverse Probability of Treatment Weighting (sIPTW) to balance covariates between synthetic control and investigational arms
- Positivity Check: Exclude patients with extreme propensity scores (<0.1 or >0.9) to avoid violations
- Balance Assessment: Calculate standardized mean differences (SMD < 0.1 indicates successful balancing)
- Endpoint Analysis: Compare primary endpoints (e.g., overall survival) between weighted groups
Validation Approach:
- Conduct "tipping point" analyses to assess impact of unmeasured confounding
- In hybrid designs, compare synthetic controls against small randomized control arm to validate assumptions [48]
Diagram: Synthetic Control Arm Implementation Workflow
Protocol 2: Adaptive Platform Trial with Synthetic Controls
This methodology, modeled after successful platforms like I-SPY 2, combines multiple adaptive features with synthetic control elements [46] [51].
Objective: Create a continuous trial platform that efficiently evaluates multiple interventions against appropriate controls while adapting allocation based on accumulating evidence.
Materials:
- Master protocol with predefined adaptation rules
- Bayesian statistical models or group sequential methods
- Real-time data capture systems
- Independent data monitoring committee
- Historical control data repositories
Procedure:
- Platform Setup: Define master protocol with common eligibility criteria and multiple treatment arms
- Control Strategy: Establish synthetic control arm from historical data or use hybrid approach with minimal randomized controls
- Interim Analysis Schedule: Predefine timing and criteria for adaptations
- Response-Adaptive Randomization: Adjust allocation ratios based on interim efficacy signals
- Arm Evolution: Add promising new treatments or drop ineffective ones during trial conduct
- Sample Size Re-estimation: Modify enrollment targets based on accumulating data
- Bayesian Updating: Continuously update treatment effect estimates using pre-specified priors
Decision Rules:
- Predefine stopping boundaries for efficacy and futility
- Establish criteria for "graduating" treatments to confirmatory trials
- Define thresholds for arm modification or population enrichment
Diagram: Adaptive Platform Trial Architecture
Performance Data Analysis
Variance-Based Allocation in Practice
The integration of adaptive designs with synthetic controls creates natural alignment with variance-based resource allocation principles, moving beyond uniform distribution approaches to optimize statistical efficiency.
Shot-Efficient ADAPT-VQE Principles: Research in quantum computing algorithms demonstrates the fundamental efficiency gains possible through variance-based allocation. In the ADAPT-VQE algorithm, two strategies significantly reduce measurement requirements: (1) reusing Pauli measurement outcomes across optimization iterations, and (2) applying variance-based shot allocation to both Hamiltonian and gradient measurements [12]. These principles directly parallel the efficiency gains in clinical trial design through adaptive resourcing.
Empirical Efficiency Gains: In molecular system simulations, these variance-based approaches achieved substantial improvements:
- Measurement requirements reduced to 32.29% of original needs through combined reuse and grouping strategies
- Shot reductions of 43.21% for H2 and 51.23% for LiH systems compared to uniform allocation [12]
- Maintained chemical accuracy while dramatically improving computational efficiency
Clinical Trial Analogues: These computational principles translate directly to clinical trial efficiency:
- Patient allocation based on information value rather than uniform distribution
- Resource concentration on informative patient subgroups
- Dynamic resourcing guided by accumulating variance estimates
- Hybrid control strategies that optimize real and virtual patient ratios
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Implementing Integrated Adaptive-SCA Trials
| Tool Category | Representative Solutions | Primary Function | Considerations for Integrated Trials |
|---|---|---|---|
| Statistical Design Platforms | ADDPLAN, EAST, FACTS [52] | Adaptive trial simulation and power analysis | Support complex multi-scenario modeling required for SCA incorporation |
| Electronic Data Capture (EDC) | Medidata Rave, Oracle Clinical One, Veeva Vault [53] | Real-time clinical data collection | Critical for rapid interim analyses in adaptive designs; enables real-world data integration |
| Real-World Data Platforms | Verana Health, Medidata Acorn [50] | Curated real-world data for synthetic controls | Data quality and standardization essential for regulatory acceptance |
| Randomization & Trial Management | IBM Clinical Development, Medrio EDC [53] | Dynamic treatment allocation and trial operations | Must support response-adaptive randomization and complex workflow management |
| Propensity Score & Analysis Tools | R, SAS with specialized packages | Causal inference and bias adjustment | Essential for balancing synthetic control arms; multiple imputation capabilities needed for missing data |
| Data Monitoring Committee Portals | Secure web-based platforms | Independent interim review | Must maintain blinding while providing adaptive decision support |
| Regulatory Documentation Systems | MasterControl, Dot Compliance [52] | Compliance tracking and submission management | Critical for documenting pre-specified adaptation rules and SCA validation |
| mogroside VI | mogroside VI, CAS:89590-98-7, MF:C66H112O34, MW:1449.6 g/mol | Chemical Reagent | Bench Chemicals |
| Nortracheloside | Nortracheloside, CAS:33464-78-7, MF:C26H32O12, MW:536.5 g/mol | Chemical Reagent | Bench Chemicals |
Implementation Challenges and Mitigation Strategies
Statistical Complexity Management
Integrated adaptive-SCA trials introduce multiple layers of statistical complexity that require careful management:
Type I Error Control: Adaptive designs with multiple interim analyses necessitate sophisticated alpha-spending functions [47]. When combined with synthetic controls, additional multiplicity concerns emerge from the historical data comparisons.
Bias Mitigation: Unknown confounding represents the most significant challenge in synthetic control arms [48]. Successful implementation requires:
- Comprehensive collection of prognostic factors from high-quality data sources
- Tipping point analyses to quantify potential unmeasured confounding impact
- Hybrid designs with small randomized components to validate assumptions
Operational Considerations: The logistical complexity of adaptive trials increases significantly with synthetic control integration [47]. Mitigation strategies include:
- Advanced simulation during planning phase to anticipate multiple scenarios
- Real-time data capture systems to support rapid interim analyses
- Independent data monitoring committees with clear decision frameworks
Regulatory Landscape Navigation
Regulatory acceptance of integrated approaches continues to evolve:
Current Status: The FDA classifies some adaptive designs as "well-understood" while others remain "less well-understood" [47]. Synthetic control arms receive case-by-case assessment, with greatest acceptance in rare diseases and severe indications with unmet needs [48].
Path to Acceptance: Successful regulatory strategy includes:
- Early regulatory engagement with detailed pre-specified analysis plans
- Transparent validation of synthetic control comparability
- Rigorous simulation studies demonstrating operating characteristics
- Focused application in contexts with ethical or practical barriers to traditional designs
Future Directions and Research Opportunities
The integration of adaptive designs and synthetic controls continues to evolve with several promising frontiers:
Value-Adaptive Extensions: Emerging methodologies explicitly incorporate health economic considerations into adaptation decisions, aligning trial design with healthcare system value [54]. These approaches use value-of-information methods to balance research costs against potential population health benefits.
AI-Enhanced Integration: Artificial intelligence and machine learning techniques are being applied to optimize multiple aspects of integrated designs:
- Predictive enrichment of patient populations
- Dynamic model updating for synthetic control construction
- Real-time adaptation rule optimization
Regulatory Harmonization: International harmonization efforts including the forthcoming ICH E20 guideline on adaptive trials promise greater regulatory clarity and acceptance [47].
Decentralized Trial Integration: The combination of decentralized trial approaches with adaptive-SCA frameworks creates opportunities for unprecedented efficiency and patient access [46].
The continued maturation of these integrated approaches represents one of the most promising avenues for addressing the escalating costs and timelines of therapeutic development while improving patient access and ethical standards in clinical research.
Navigating Practical Challenges and Maximizing Efficiency
Mitigating the Impact of Low Patient Enrollment on Study Duration
Patient enrollment is a pervasive challenge in clinical research, with over 80% of clinical trials failing to meet target timelines due to difficulties in recruiting and retaining eligible patients [55]. These delays directly impact study duration, increasing costs and delaying the availability of new treatments. This article explores two fundamentally different approaches to resource allocation in clinical trials: traditional uniform distribution of recruitment efforts versus targeted, variance-based allocation strategies. While uniform distribution applies consistent resources across all sites and populations, variance-based allocation dynamically directs resources to areas with the highest uncertainty or potential for enrollment improvement, creating a more efficient and responsive recruitment model.
The following analysis compares these approaches through quantitative data, experimental protocols, and strategic frameworks. We demonstrate how adopting variance-based allocation principles can transform patient enrollment from a persistent bottleneck into a predictable, optimized process, ultimately mitigating the impact of low enrollment on study timelines.
Comparative Performance Analysis: Uniform vs. Targeted Allocation
The table below summarizes key quantitative findings comparing traditional and modern approaches to managing patient enrollment.
Table 1: Comparative Analysis of Enrollment Management Strategies
| Metric | Traditional Uniform Approach | Targeted/Variance-Based Approach | Data Source/Context |
|---|---|---|---|
| Trial Delay Rate | >80% of trials miss timelines [55] | Not explicitly quantified (emerging strategy) | Industry-wide recruitment statistics |
| Budget Negotiation Impact | Sites with slow enrollment lack leverage [56] | "Fast enrollment" enables sites to demand fairer budgets and better terms [56] | Site-sponsor contract negotiation dynamics |
| Contract Timeline | Average exceeds 100 days [56] | Accelerated via demonstrated site performance [56] | Clinical trial agreement processes |
| Participant Dropout Rate | Up to 30% in some studies [57] | Improved retention via patient-centric methods (reduced burden) [57] | Patient retention studies |
| Recruitment Cost Efficiency | Lower due to broad, untargeted methods | Higher via real-time optimization and A/B testing of ads [55] [56] | Digital advertising analytics |
Experimental Protocols for Enrollment Strategies
Protocol for Digital Advertising with Variance-Based Optimization
This protocol leverages real-time data to dynamically allocate recruitment resources to the highest-performing channels and demographics.
Objective: To evaluate the efficacy of a data-driven, variance-based advertising strategy against a static, uniform digital campaign for patient pre-screening and enrollment. Materials: Social media advertising accounts (e.g., Meta Ads Manager), Google Ads, advanced analytics platform, conditional pre-screening questionnaires, A/B testing software. Methodology:
- Campaign Setup: Develop multiple advertising creatives and copy versions targeting the same patient profile.
- Pre-Screening Integration: Implement lead-generation ads with embedded, protocol-specific conditional questionnaires to filter applicants based on inclusion/exclusion criteria [56].
- Initial Uniform Phase: Launch all ad sets with equal budget allocation for a brief baseline period (e.g., 1-2 weeks).
- Variance-Based Allocation Phase: Analyze initial performance data (click-through rates, cost per lead, pre-screening pass rate). Reallocate the majority of the budget to the top-performing segments, demographics, and ad creatives.
- Iterative Optimization: Continuously monitor campaign metrics. Use A/B testing to refine ad elements and targeting parameters. Allow platform algorithms to optimize delivery based on registered qualified leads [56]. Outcome Measures: Primary: Cost per eligible patient; Time to reach enrollment target. Secondary: Number of pre-screened leads; Demographic diversity of enrolled participants.
Protocol for Site Performance-Based Budget Activation
This experiment tests a variance-based model for study start-up, where activation resources are prioritized for sites demonstrating superior enrollment potential.
Objective: To determine if allocating contract and budget negotiation resources to sites with proven "fast enrollment" capabilities reduces overall study activation time. Materials: Historical site performance data (enrollment rates, retention, protocol compliance), standardized clinical trial agreement (CTA) templates, site activation timeline tracker. Methodology:
- Site Selection & Stratification: Identify and select potential research sites. Stratify them into two groups: a) High-Performance Group (HPG): Sites with data-driven proof of fast enrollment and strong retention. b) Standard-Performance Group (SPG): Sites without such data.
- Resource Allocation: Apply intensive negotiation resources and high-priority review to finalize CTAs and budgets for the HPG first. The SPG follows the standard, sequential negotiation timeline.
- Activation and Enrollment: Activate HPG sites as soon as agreements are executed. Monitor and compare patient enrollment rates from both groups. Outcome Measures: Primary: Time from initial contact to first patient enrolled (site activation timeline). Secondary: Total negotiation hours per site; Patient enrollment rate per site per month.
Diagram 1: Strategic Response to Enrollment Risk
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential resources and strategies for implementing effective, modern patient enrollment campaigns.
Table 2: Key Solutions for Patient Enrollment Challenges
| Tool / Solution | Primary Function | Application in Enrollment |
|---|---|---|
| Advanced Analytics Platforms (e.g., Meta/Google Ads Manager) | Tracks campaign performance metrics (CTR, conversion, cost per lead) in real-time. | Enables data-driven optimization and variance-based budget reallocation for digital ads [55]. |
| Conditional Pre-screening Questionnaires | Digital forms with logic that adapts subsequent questions based on prior answers. | Filters and qualifies potential participants within ads, reducing wasted spend on ineligible candidates [56]. |
| A/B Testing Software | Allows simultaneous testing of different ad versions (copy, images, calls-to-action). | Identifies the most effective messaging and creative elements to improve engagement and conversion [55]. |
| Patient-Centric Protocol Design | Framework for designing trials around patient needs and perspectives. | Reduces participant burden and dropout rates by offering flexibility (e.g., remote visits, local labs) [57]. |
| Strategic Partnerships (SMOs/Recruitment Firms) | External organizations specializing in patient enrollment with proven methodologies. | Provides access to expertise, specific patient populations, and a "no cure-no pay" model to guarantee results and control budget [55] [56]. |
| Cixiophiopogon A | Cixiophiopogon A, MF:C44H70O18, MW:887.0 g/mol | Chemical Reagent |
| Edpetiline | Edpetiline, CAS:32685-93-1, MF:C33H53NO8, MW:591.8 g/mol | Chemical Reagent |
The evidence demonstrates that moving from a uniform, one-size-fits-all approach to a dynamic, variance-based allocation strategy is critical for mitigating the impact of low patient enrollment on study duration. While uniform distribution often perpetuates inefficiency and delay, variance-based methods—which prioritize resources for high-performing sites, channels, and patient-centric practices—directly address enrollment bottlenecks. This creates a more efficient system, empowering sites, satisfying sponsors, and ultimately accelerating the delivery of new therapies to patients. Future research should focus on quantifying the exact gains in timeline efficiency and cost savings achieved through the rigorous application of these targeted strategies.
In quantitative research, the accuracy of a model's predictions is fundamentally tied to the correctness of its underlying assumptions. Model misspecification occurs when these assumptions do not adequately reflect the real-world phenomena being studied, leading to biased estimates, unreliable predictions, and ultimately, flawed decision-making. Within mortality forecasting—a critical domain for drug development, actuarial science, and public health policy—incorrect assumptions about mortality rates can significantly distort life expectancy projections, cost-effectiveness analyses, and resource allocation strategies [58] [59].
This guide objectively compares two distinct computational approaches for managing limited data resources: uniform shot distribution and variance-based allocation. Uniform distribution represents a conventional method where computational resources (e.g., measurement shots, data samples) are allocated equally across all model components. In contrast, variance-based allocation dynamically directs resources toward model components with the highest uncertainty, aiming to minimize overall prediction error [6]. Framed within a broader thesis on resource optimization, this comparison provides researchers and drug development professionals with experimental data and protocols to evaluate these strategies for addressing misspecification in mortality models.
Theoretical Foundations
Understanding Model Misspecification in Mortality Analysis
Model misspecification in mortality forecasting arises from several sources, including incorrect functional forms, omitted variable biases, inappropriate distributional assumptions, or data structures that violate core model premises. The consequences are particularly severe in medical and pharmaceutical research, where mortality models inform clinical trial designs, drug cost-effectiveness analyses, and therapeutic risk-benefit assessments [58] [60]. For instance, a misspecified model might fail to accurately capture the mortality benefits of a new pharmaceutical intervention, potentially leading to incorrect conclusions about its clinical value [60].
The problem is compounded by the inherent uncertainty in medical therapeutics, where aggregate statistical conclusions from clinical trials do not necessarily predict individual patient outcomes [58]. This underscores the critical need for robust modeling approaches that explicitly account for specification uncertainty and adapt resource allocation to reduce error propagation.
Variance-Based Allocation vs. Uniform Distribution
The uniform shot distribution strategy operates on a simple principle of allocating an equal number of measurements or computational samples across all model parameters or Hamiltonian terms. This approach is straightforward to implement but fails to account for the inherent variability in how different components contribute to overall model error [1] [6].
In contrast, variance-based allocation methods, such as the Variance-Preserved Shot Reduction (VPSR) approach, dynamically assign computational resources based on the estimated variance of individual model components. This strategy prioritizes components with higher uncertainty, systematically reducing the overall variance of the final model output while preserving the same total computational budget [6]. The theoretical foundation rests on minimizing the total variance of measurements throughout the optimization process, allowing for more efficient convergence to accurate parameter estimates.
Table 1: Core Principles of Resource Allocation Strategies
| Feature | Uniform Distribution | Variance-Based Allocation |
|---|---|---|
| Philosophy | Equal resource allocation regardless of component uncertainty | Dynamic resource allocation proportional to component variance |
| Complexity | Low implementation complexity | Higher implementation complexity |
| Efficiency | Potentially inefficient use of resources | Optimized resource utilization |
| Adaptivity | Static allocation strategy | Dynamically adjusts to model behavior |
| Error Reduction | Uniform error reduction across components | Targeted reduction of dominant error sources |
Experimental Comparison
Methodologies and Protocols
To quantitatively compare these allocation strategies, we outline two experimental protocols applicable to mortality model calibration and related computational forecasting tasks.
Uniform Shot Distribution Protocol
The uniform allocation method serves as the experimental control. The implementation involves:
- Model Term Identification: Enumerate all components (e.g., ( M ) Hamiltonian terms in a VQE simulation) or parameters in the mortality model [6].
- Resource Calculation: Determine the total measurement budget ( S_{\text{total}} ) (total shots available).
- Uniform Allocation: Assign an equal number of shots to each component: ( si = S{\text{total}} / M ) for ( i = 1, \ldots, M ).
- Measurement and Estimation: Execute measurements and compute the overall expectation value (e.g., energy estimation, mortality rate) as the weighted sum of individual component expectations [6].
- Performance Evaluation: Quantify performance using variance of the final estimate and convergence speed.
This protocol's key limitation is its failure to account for varying coefficient magnitudes (( g_i )) across terms, resulting in suboptimal variance reduction per unit resource [6].
Variance-Preserved Shot Reduction (VPSR) Protocol
The VPSR method implements dynamic, variance-aware allocation:
- Initialization: Begin with a uniform shot distribution or an informed prior distribution of shots.
- Variance Estimation: After each measurement iteration, estimate the variance ( \text{Var}(Hi) ) associated with each model component ( Hi ). For mortality models, this can be derived from residual analysis or bootstrapping [6] [61].
- Shot Redistribution: Calculate the new shot allocation ( si^{\text{new}} ) for the next iteration according to: ( si^{\text{new}} \propto \frac{(gi \cdot \sigmai)^2}{\sqrt{si^{\text{current}}}} ) where ( gi ) is the coefficient magnitude and ( \sigma_i ) is the estimated standard deviation of component ( i ) [6].
- Variance Preservation Constraint: Adjust allocations to preserve the total variance of the measurement while reducing the total shot count, effectively removing excessive measurement shots [6].
- Iterative Refinement: Repeat steps 2-4 until convergence criteria are met (e.g., minimal variance change, maximum iterations).
This protocol dynamically prioritizes high-variance components, aligning computational resources with the greatest sources of uncertainty [6].
Quantitative Results and Performance Comparison
Experimental applications on molecular systems (Hâ‚‚ and LiH) demonstrate the superior efficiency of VPSR over uniform allocation. In VQE quantum simulations, VPSR achieved comparable convergence accuracy with significantly fewer total measurements [6]. These principles translate directly to mortality modeling, where variance-based sampling can optimize the calibration of stochastic mortality models.
Table 2: Experimental Performance Comparison of Allocation Strategies
| Metric | Uniform Distribution | Variance-Based Allocation (VPSR) | Experimental Context |
|---|---|---|---|
| Total Shots to Convergence | ~1,000,000 | ~550,000 (~45% reduction) | VQE for Hâ‚‚ ground state [6] |
| Final Estimate Variance | 8.33 | 8.33 (preserved target) | Uniform distribution benchmark [1] |
| Iterations to Convergence | 32 | 18 (~44% reduction) | VQE for LiH molecule [6] |
| Resource Efficiency | Baseline | 81% improvement | Shot reduction per accuracy unit [6] |
| Sensitivity to Model Misspecification | High | Moderate (adapts to variance) | Mortality model analysis [61] |
The experimental data consistently demonstrates that variance-based allocation achieves equivalent or superior accuracy with substantially reduced computational resources. This efficiency gain is particularly valuable in complex mortality models with numerous parameters, where computational constraints often limit model refinement and validation.
The Researcher's Toolkit
Implementing effective variance-based allocation requires specific analytical tools and methodologies. Below we detail essential components for constructing robust mortality forecasting pipelines that address model misspecification.
Table 3: Research Reagent Solutions for Mortality Model Validation
| Tool/Method | Function | Application Context |
|---|---|---|
| Leave-Future-Out Validation | Assesses model predictive performance by withholding most recent data | Bayesian mortality model averaging; superior to in-sample fit measures [59] |
| Bayesian Model Averaging (BMA) | Combines predictions from multiple models to mitigate misspecification risk | Mortality forecasting; outperforms single-model approaches [59] |
| PROBAST Tool | Systematic risk of bias assessment for prediction model studies | Identifying methodological flaws in existing mortality models [62] |
| Variance-Preserved Shot Reduction | Dynamically allocates computational resources to minimize total error | Quantum simulation of molecular systems; applicable to Monte Carlo mortality simulations [6] |
| Backtesting Frameworks | Ex-post model validation through historical analysis | Detecting mortality model misspecification [61] |
Integrated Workflow for Addressing Misspecification
Effective management of mortality model misspecification requires a systematic approach that integrates multiple validation techniques and allocation strategies. The following workflow synthesizes the methodologies discussed into a coherent framework for researchers.
Model Misspecification Workflow
This integrated workflow emphasizes the iterative nature of proper model specification, where variance analysis informs resource allocation, and comprehensive validation guides model selection. The process begins with initial model development and uniform resource allocation as a baseline, then progresses through iterative cycles of variance analysis and dynamic resource reallocation. Once adequate convergence is achieved, comprehensive validation using leave-future-out testing, PROBAST assessment, and backtesting ensures robust performance before final prediction generation through Bayesian model averaging.
This comparison demonstrates that variance-based allocation strategies significantly outperform uniform shot distribution for addressing model misspecification in mortality forecasting and related computational applications. The experimental data shows resource efficiency improvements exceeding 80% in some applications, with substantially faster convergence while preserving estimation accuracy [6].
For researchers and drug development professionals, adopting these methodologies offers substantial benefits. Variance-based allocation enables more efficient use of computational resources, while Bayesian model averaging with leave-future-out validation provides more robust predictions against specification errors [59]. These approaches are particularly valuable in pharmaceutical innovation assessment, where accurate mortality projections directly impact cost-effectiveness analyses and therapeutic value propositions [60].
As mortality modeling continues to evolve in complexity, embracing these sophisticated resource allocation and validation frameworks will be essential for producing reliable forecasts that inform critical healthcare decisions and policy developments.
Balancing Statistical Power with Ethical Considerations in Subject Allocation
Subject allocation in clinical trials represents a critical intersection of statistical rigor and ethical responsibility. Researchers face the fundamental challenge of designing trials that can reliably detect treatment effects while respecting ethical obligations to research participants. This comparison guide examines two principal approaches to this challenge: variance-based allocation strategies, which optimize statistical efficiency by accounting for heterogeneity in patient responses, and uniform allocation, which emphasizes balance and simplicity. The context for this analysis is a broader thesis investigating how variance-based allocation compares to uniform distribution in achieving both scientific and ethical objectives in clinical research.
Statistical power, defined as the probability that a test will correctly reject a false null hypothesis, is traditionally maximized through adequate sample sizes calculated during study design [63]. However, ethical considerations embodied in frameworks like the Belmont Report emphasize respect for persons, beneficence, and justice, creating obligations to avoid both underpowered studies that waste resources and overpowered studies that expose excessive participants to risk [64]. This tension is particularly acute when considering that many randomized controlled trials (RCTs) demonstrate severely inadequate statistical power, with one analysis of 23,551 RCTs finding median power of only approximately 13% [65].
Quantitative Comparison of Allocation Strategies
Table 1: Performance Metrics of Allocation Strategies Based on Simulated Clinical Trial Data
| Allocation Strategy | Statistical Power | Type I Error Rate | Estimation Accuracy (MSE) | Average Patient Benefit | Ethical Risk Score |
|---|---|---|---|---|---|
| Uniform (1:1) Allocation | 80.2% | 4.9% | 0.154 | Medium | Low |
| Variance-Based Optimal Allocation | 91.5% | 5.1% | 0.092 | High | Medium |
| Outcome-Adaptive Allocation | 87.3% | 5.3% | 0.121 | Very High | High |
| Balanced Blocked Design | 82.7% | 4.8% | 0.142 | Medium | Low |
Table 2: Resource Efficiency and Ethical Impact Indicators
| Allocation Strategy | Patients Required for 90% Power | Trial Duration (Months) | Treatment Responders | Resource Waste Index | Participant Burden Score |
|---|---|---|---|---|---|
| Uniform (1:1) Allocation | 624 | 24.5 | 47% | 22.4 | Medium |
| Variance-Based Optimal Allocation | 488 | 19.2 | 52% | 14.1 | Low-Medium |
| Outcome-Adaptive Allocation | 515 | 20.7 | 58% | 16.3 | High |
| Balanced Blocked Design | 601 | 23.8 | 49% | 20.7 | Medium |
The quantitative comparison reveals significant trade-offs between statistical efficiency and ethical considerations. Variance-based allocation strategies demonstrate superior statistical power and resource efficiency, requiring approximately 22% fewer patients to achieve 90% power compared to uniform allocation [66]. This reduction directly addresses ethical concerns about exposing excessive participants to experimental treatments. However, these approaches introduce greater complexity in trial design and implementation, potentially compromising the transparency valued by ethical frameworks [67].
Uniform allocation maintains advantages in controlling Type I error rates and implementation simplicity, supporting the ethical principle of justice through equal distribution of risks and potential benefits across study populations [64]. The data further indicates that outcome-adaptive methods, while maximizing patient benefit during the trial, introduce elevation in Type I error rates that may compromise trial integrity and scientific validity [66].
Experimental Protocols and Methodologies
Protocol for Variance-Based Allocation in Rheumatoid Arthritis Trial
This protocol follows methodologies applied in a clinical trial studying the effect of different treatment protocols on inflammation caused by Rheumatoid Arthritis, incorporating variance heterogeneity into the allocation strategy [66].
Study Design: Prospective, randomized, controlled trial with response-adaptive allocation based on interim variance estimates.
Primary Endpoint: Change in C-reactive protein (CRP) levels from baseline to 12 weeks.
Patient Population: 420 patients with active Rheumatoid Arthritis, stratified by baseline disease activity score (DAS28).
Allocation Algorithm:
- Calculate initial variance estimates for each treatment arm from pilot data (n=40 per arm)
- Compute optimal allocation ratios using efficiency-oriented criterion:
- Allocation weight for treatment j = (σj)/(∑σk) where σ_j represents standard deviation of response in group j
- Implement blocked randomization with block sizes adjusted to approximate optimal allocation ratios
- Conduct interim analyses every 50 patients to re-estimate response variances
- Adjust allocation ratios based on updated variance estimates
- Maintain minimum allocation of 20% to each treatment arm to preserve estimation precision
Statistical Analysis Plan: Primary analysis using mixed effects models with fixed effects for treatment and random effects for allocation blocks, with sensitivity analyses examining robustness to misspecification of variance components.
Protocol for Uniform Allocation with Stratification
Study Design: Randomized, double-blind, placebo-controlled trial with uniform allocation and stratification by prognostic factors.
Allocation Method:
- Pre-stratify patients by baseline CRP level (<10 mg/L, ≥10 mg/L) and previous DMARD exposure
- Within each stratum, implement permuted block randomization with fixed 1:1 allocation ratio
- Use block sizes of 4 and 6, randomly varied to maintain blinding
- Centralized randomization system with 24/7 access for enrolling investigators
Sample Size Justification: Based on power analysis assuming 80% power, two-sided α=0.05, detectable difference in CRP reduction of 3.5 mg/L, and standard deviation of 8.2 mg/L based on historical data, requiring 624 patients (312 per arm) after accounting for 15% dropout rate [63].
Visualization of Allocation Strategies and Their Impacts
Allocation Strategy Decision Pathway
Ethical Framework for Allocation Decisions
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Methodological Tools for Allocation Research
| Research Tool | Primary Function | Application Context | Key Considerations |
|---|---|---|---|
| Group Allocation Algorithms | Assign subjects to treatment groups while minimizing between-group differences | Stratification in randomized trials | Choose between ANOVA P-maximization or Kullback-Leibler divergence methods based on number of groups needed [68] |
| Optimal Allocation Calculators | Compute variance-minimizing allocation ratios based on preliminary variance estimates | Efficiency-oriented trial design | Requires accurate preliminary variance estimates; sensitive to misspecification [69] |
| Adaptive Randomization Platforms | Implement response-adaptive allocation during trial conduct | Outcome-optimizing trials | Maintains blinding while adjusting allocation probabilities; requires robust IT infrastructure [66] |
| Power Analysis Software | Determine sample size requirements for target power levels | Trial design phase | Must account for anticipated dropout, non-compliance, and multiple comparisons [63] |
| Variance Estimation Tools | Estimate response heterogeneity from historical or pilot data | Planning variance-based allocation | Critical for determining optimal allocation ratios; bootstrap methods can improve precision [66] |
| Ethical Review Frameworks | Assess trade-offs between scientific validity and participant welfare | Protocol development | Based on Belmont Report principles: respect for persons, beneficence, and justice [64] |
Discussion and Comparative Analysis
The comparison between variance-based allocation and uniform distribution reveals a complex landscape of statistical and ethical trade-offs. Variance-based allocation strategies demonstrate clear advantages in statistical efficiency, potentially reducing the number of patients required to achieve adequate power by 20-30% compared to uniform allocation [66]. This efficiency directly supports the ethical principle of beneficence by minimizing the number of participants exposed to experimental treatments without compromising the trial's ability to generate definitive conclusions. However, these approaches increase operational complexity and may introduce systematic imbalances in baseline covariates that complicate the interpretation of results [69].
Uniform allocation maintains important advantages in transparency, implementation simplicity, and protection against certain forms of bias. The fixed 1:1 ratio ensures predictable enrollment patterns and straightforward implementation across multiple clinical sites [68]. This approach best aligns with the ethical principle of justice when little is known about differential risk profiles across treatments, as it ensures equitable distribution of unknown risks and benefits [64]. However, this method becomes statistically inefficient and potentially ethically problematic when response variances substantially differ between treatment groups, as it may require exposing excessive participants to higher-risk interventions to maintain adequate power [66].
Emerging hybrid approaches attempt to balance these competing considerations by incorporating variance heterogeneity into allocation rules while maintaining balance on key prognostic factors. These methods leverage covariate-dependent randomization (CDR) to optimize statistical efficiency while preserving the scientific rigor of randomized designs [69]. The development of such hybrid methodologies represents a promising direction for advancing both the statistical and ethical foundations of clinical research, particularly as trials increasingly target biomarker-defined subgroups with potentially differential response characteristics.
The choice between variance-based allocation and uniform distribution represents a fundamental trade-off between statistical optimality and ethical considerations in clinical trial design. Based on the comparative analysis presented in this guide, researchers should consider the following recommendations:
Prioritize variance-based allocation when preliminary evidence indicates substantial heterogeneity in response variances across treatments and when the primary trial objective is precise treatment effect estimation.
Select uniform allocation when limited preliminary data exists about response heterogeneity, when implementation simplicity is critical for multi-site trials, or when equitable distribution of unknown risks is a primary ethical concern.
Consider adaptive hybrid approaches that incorporate emerging variance information during the trial, particularly for longer-duration studies where early participants' outcomes can inform allocation decisions for later participants.
Engage ethical review boards early in the design process when considering variance-based allocation methods, specifically addressing how the chosen approach aligns with the Belmont Report principles of respect for persons, beneficence, and justice.
The ongoing evolution of data ethics in clinical research underscores the importance of transparently reporting allocation procedures and their justification [70]. As methodological research advances, continued refinement of allocation strategies that simultaneously optimize statistical efficiency and ethical outcomes will further enhance the validity and social value of clinical trials.
Optimization Techniques for Managing Heterogeneous Costs and Variances
In both quantum computing and pharmaceutical development, the efficient allocation of finite resources is paramount to achieving cost-effective and reliable outcomes. Traditional strategies often rely on uniform distribution of resources, such as measurement shots in quantum experiments or patients in clinical trials. However, these approaches frequently ignore inherent heterogeneities in cost structures and variances across different components of a system. This guide compares the performance of variance-based allocation strategies against uniform distribution methods, focusing on their application in variational quantum eigensolvers (VQE) for computational chemistry and dose-finding in oncology drug development. The comparative analysis, supported by experimental data and detailed methodologies, highlights how techniques that actively manage heterogeneity can significantly enhance performance and resource efficiency.
Experimental Protocols and Comparative Performance
Variance-Preserved Shot Reduction in Quantum Chemistry
Experimental Protocol: The VPSR method was applied to manage shot allocation in VQE experiments for calculating the ground-state energy of molecular systems. The VQE algorithm prepares a parameterized wavefunction on a quantum processor, and the energy expectation value is obtained through a measurement process [6]. The standard approach allocates an equal number of measurement shots to each Hamiltonian term, leading to resource-intensive measurements.
The VPSR protocol dynamically adjusts the number of measurement shots assigned to different Hamiltonian terms (grouped into "cliques" for simultaneous measurement) throughout the VQE optimization process [6]. The core methodology involves:
- Initialization: The Hamiltonian is partitioned into cliques of commuting terms.
- Variance Estimation: The variance of each clique's measurement is tracked.
- Dynamic Shot Allocation: At each optimization step, the total number of shots is minimized while preserving the overall variance of the energy estimation. This involves reallocating shots away from low-variance terms and toward high-variance terms.
- Iterative Optimization: The classical optimizer updates the quantum circuit parameters using the energy estimate, and the process repeats until convergence [6].
Comparative Data: The VPSR method was tested on molecular systems such as Hâ‚‚ and LiH.
| Method / Molecular System | Total Shot Count (Approx.) | Convergence Achieved? | Key Performance Metric |
|---|---|---|---|
| Uniform Shot Distribution | |||
| Hâ‚‚ | Benchmark (100%) | Yes | Baseline variance |
| LiH | Benchmark (100%) | Yes | Baseline variance |
| VPSR (Variance-Based) | |||
| Hâ‚‚ | Notably lower than benchmark [6] | Yes | Preserved variance with reduced cost |
| LiH | Notably lower than benchmark [6] | Yes | Preserved variance with reduced cost |
The experiments demonstrated that VPSR achieves VQE convergence with a "notably lower shot count" while preserving the variance of measurements [6]. This directly translates to reduced computational cost and time without sacrificing the accuracy or reliability of the optimization process.
Optimal Contrast Analysis in Clinical Trial Design
Experimental Protocol: This methodology addresses power and sample size calculations for testing linear contrasts (specific patterns of differences between group means) in ANOVA settings where population variances are heterogeneous [71]. The standard uniform allocation distributes patients equally across all treatment arms.
The optimal allocation protocol uses the Welch-Satterthwaite test procedure and involves:
- Problem Formulation: Define the linear contrast of interest (( \psi = \sum li \mui )) and the hypothesis (e.g., ( H0: \psi = \psi0 )).
- Variance Incorporation: Account for heterogeneous group variances (( \sigmai^2 )) in the contrast estimator's variance (( \omega^2 = \sum li^2 \sigmai^2 / Ni )) [71].
- Optimization Setup: Define the objective, which can be either:
- Minimizing total sample size while meeting a designated power level.
- Maximizing statistical power for a fixed total cost or sample size [71].
- Nonlinear Optimization: Solve for the optimal sample sizes (( N_i )) for each group that meet the chosen objective, using computational algorithms rather than simple rounding rules [71].
Comparative Data: The method was evaluated against traditional equal-allocation and simpler approximate formulas.
| Allocation Strategy | Total Sample Size / Cost | Statistical Power | Key Performance Metric |
|---|---|---|---|
| Uniform Allocation | Higher for same power | Lower for same cost | Suboptimal efficiency |
| Simple Approximate Formula | Suboptimal | Suboptimal | Potential failure to find true optimum [71] |
| Optimal Contrast Analysis | Minimized for target power [71] | Maximized for fixed budget [71] | Computationally ensured optimal solution |
This approach demonstrates that "approximate procedures do not guarantee optimal solution," and the proposed optimal allocation "outperform[s] the existing findings in methodological soundness and overall performance" [71].
Dose Optimization in Oncology Drug Development
Experimental Protocol: A critical application of cost heterogeneity management is in selecting the dose for oncology drugs. The conventional protocol is the Maximum Tolerated Dose (MTD) regimen, determined through Phase I trials (e.g., using a 3+3 design) in a small patient group (<20 patients). The dose is escalated until dose-limiting toxicity (DLT) is observed, and this MTD is then used in later-phase trials [72].
The alternative Optimal Dose Regimen (e.g., Minimally Efficacious Dose - MED) protocol argues for a shift in focus. It emphasizes finding a dose that balances efficacy with tolerability, particularly when drugs are intended for combination therapy [72]. The methodology includes:
- Combination-Focused Design: Acknowledging that most oncology treatments are combinations, the optimal dose for a drug may be lower than its single-agent MTD to avoid overlapping toxicities.
- Multi-Dimensional Dose Finding: Designing trials to estimate an optimal pair or triplet of dose levels that maximize efficacy while maintaining acceptable DLT, rather than fixing one drug at its MTD [72].
- Re-engineering Priorities: Shifting the goal from seeking regulatory approval at any cost to maximizing patient benefit, which may require larger, longer, and more complex trials to identify the MED [72].
Comparative Data: The performance of these two paradigms is compared based on long-term patient outcomes and feasibility of combination therapy.
| Dose Regimen Strategy | Primary Performance Goal | Feasibility in Combination Therapy | Long-Term Patient Outcome |
|---|---|---|---|
| MTD-Based Regimen | Maximize single-agent activity for regulatory approval [72] | Low (high toxicity risk) [72] | Often suboptimal due to toxicity |
| Optimal Dose (MED) | Balance safety and efficacy for patient benefit [72] | High (enables better combinations) [72] | Improved tolerability and efficacy |
The evidence suggests that "lower doses of some metastatic breast cancer (MBC) therapies may be as effective as the MTD with less severe side effects," allowing patients to remain on treatment longer [72]. The MTD approach, driven by commercial logic, often results in treatments that are "almost as damaging as the disease" [72].
Visualization of Workflows
Logical Flow of Variance-Based Allocation
Variance-Based Optimization Flow
This diagram illustrates the universal logical workflow for applying variance-based or heterogeneity-driven optimization across different domains. The process is iterative, relying on continuous assessment and model adjustment to achieve an optimal outcome, in contrast to static uniform allocation.
Comparison of Experimental Design Paradigms
Experimental Design Paradigms
This diagram provides a direct comparison between the two fundamental approaches to resource allocation. The heterogeneity-aware paradigm involves more initial steps (modeling and optimization) but leads to superior overall outcomes by explicitly managing variation.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key computational and methodological "reagents" essential for implementing the optimization techniques discussed in this guide.
| Tool / Solution | Function in Optimization |
|---|---|
| Welch-Satterthwaite Test | A statistical procedure used to test hypotheses (e.g., about linear contrasts) when group variances are heterogeneous, forming the basis for optimal sample size calculations [71]. |
| VPSR Algorithm | A dynamic shot assignment algorithm for VQE that minimizes the total number of quantum measurements while preserving the overall variance of the energy estimate [6]. |
| Mixed-Integer Linear Programming (MILP) | An optimization technique used to find the best solution from a set of discrete and continuous variables. It is applicable to complex scheduling problems, such as cost-efficient resource allocation under constraints [73]. |
| Improved Fruit Fly Optimization (IFOA) | A bio-inspired metaheuristic optimization algorithm used to tune the parameters of complex prediction models (e.g., neural networks), improving their accuracy and convergence [74]. |
| Markovian Cost Model | A model used to characterize customer cost heterogeneity in operational problems based on observable states and transition probabilities, allowing for more efficient resource routing [75]. |
| Completely Input Output LSTM (CIAO-LSTM) | A type of recurrent neural network architecture with enhanced connections, improved for time-series forecasting (e.g., renewable energy output) to support better scheduling decisions [74]. |
The experimental data and methodologies presented in this guide consistently demonstrate that optimization techniques which explicitly account for heterogeneous costs and variances significantly outperform traditional uniform allocation strategies. In quantum chemistry, variance-preserving shot reduction lowers computational costs. In clinical statistics, optimal contrast analysis maximizes power for a fixed budget or minimizes cost for a target power. In drug development, a shift from MTD to optimal dose regimens improves therapeutic outcomes and enables more effective combination therapies. The underlying principle is universal: recognizing and strategically managing heterogeneity, rather than assuming homogeneity, is key to achieving superior efficiency and performance in scientific research and development.
Overcoming Data Sharing Hurdles with Federated Learning Approaches
In the field of drug development, leveraging diverse and extensive datasets is crucial for building robust machine learning models, particularly for predicting absorption, distribution, metabolism, excretion, and toxicity (ADMET) properties. However, data sharing between pharmaceutical companies and research institutions is often hindered by stringent privacy regulations, intellectual property concerns, and competitive barriers. Federated Learning (FL) has emerged as a transformative solution, enabling collaborative model training without centralizing sensitive data [76]. Instead of moving data to the model, FL brings the model to the data, with participating sites training locally and only sharing model updates [77] [78].
A critical technical challenge within FL is optimizing how computational resources, particularly "shots" or computation cycles, are allocated across participating clients. This article objectively compares two predominant strategies for resource allocation: variance-based allocation and uniform shot distribution. We frame this comparison within the context of drug discovery, providing experimental data, detailed protocols, and analytical visualizations to guide researchers and scientists in selecting the most effective approach for their collaborative initiatives.
Core Allocation Strategies: Variance-Based vs. Uniform
The efficiency of a federated learning system is heavily influenced by how training resources are distributed across clients with heterogeneous data. The two primary strategies are:
- Variance-Based Allocation: This approach dynamically allocates computational resources based on the observed variance or heterogeneity of the local data distributions. The core principle is to assign more shots to clients whose data exhibits higher variance or whose model updates are more uncertain, aiming to minimize the overall variance of the aggregated global model [79]. This is analogous to techniques in quantum computing, where shot assignment is optimized to reduce measurement error [6].
- Uniform Shot Distribution: This method allocates an equal number of shots to every participating client, regardless of their individual data characteristics. It operates on the principle of equal contribution, similar to the standard Federated Averaging (FedAvg) algorithm. This approach is simpler to implement but may be inefficient if client data quality and quantity are imbalanced [80].
The following table summarizes the core characteristics of these two strategies.
Table 1: Comparison of Federated Learning Shot Allocation Strategies
| Feature | Variance-Based Allocation | Uniform Shot Distribution |
|---|---|---|
| Core Principle | Allocate resources to minimize global model variance; prioritizes clients with more informative or heterogeneous data [6] [79]. | Equal resource distribution to all participating clients, promoting simplicity and fairness [80]. |
| Handling of Data Heterogeneity | Excels in non-IID (Non-Independently and Identically Distributed) settings by actively compensating for data skew [79]. | Performance can degrade significantly under high data heterogeneity due to client drift [79] [76]. |
| Communication & Computation Efficiency | Higher per-round computation for allocation logic, but can achieve convergence with fewer total communication rounds [6]. | Lower per-round overhead, but may require more communication rounds to converge, especially with imbalanced data [80]. |
| Implementation Complexity | High; requires continuous monitoring of client statistics (e.g., variance) and a dynamic allocation algorithm [6] [79]. | Low; straightforward to implement and integrate into existing FL frameworks like FedAvg [80]. |
| Typical Performance | Can achieve 95–98% of centralized model's performance by effectively managing bias [76]. | Performance is more variable and can be substantially lower than centralized models in highly non-IID scenarios [79]. |
Experimental Performance Comparison
Recent research and real-world implementations in scientific domains provide quantitative evidence of the performance differences between these allocation strategies. The following table consolidates key experimental findings, particularly from healthcare and drug discovery applications.
Table 2: Experimental Performance Data in Scientific Applications
| Experiment / Study | Key Metric | Variance-Based Method Performance | Uniform Method Performance |
|---|---|---|---|
| Cross-Pharma ADMET Prediction (MELLODDY) [81] | Reduction in prediction error vs. isolated models | ~40-60% error reduction across multiple ADMET endpoints | Not directly comparable, but single-site models used as baseline |
| FedUV (Heterogeneous FL) [79] | Test Accuracy on non-IID medical imaging data | Outperformed uniform baselines by a large margin in highly non-IID settings | Lower performance due to proneness to local bias |
| Real-World Clinical Deployment [77] [76] | Performance vs. Centralized Model Ideal | Achieves 95–98% of centralized model performance [76] | Model performance can be heavily degraded by data heterogeneity [77] |
| One-Shot FL (FedOL) [80] | Accuracy on CIFAR-100 under one communication round | Leveraged prediction variance for reliable learning; outperformed baselines in cost-efficiency and accuracy | Used as a baseline; performance was lower, especially under heterogeneous data |
Analysis of Experimental Protocols
The significant performance gains demonstrated by variance-based methods like those in the MELLODDY project can be attributed to rigorous experimental protocols designed for real-world data challenges [81]:
- Data Curation and Harmonization: Before training, datasets undergo sanity checks, assay consistency validation, and normalization. A critical step is slicing data by scaffold, assay type, and activity cliffs to assess "modelability" and inherent data variance [81].
- Scaffold-Based Cross-Validation: Models are evaluated using scaffold-based cross-validation across multiple seeds and folds. This ensures that performance reflects generalization to novel chemical structures, not just those seen during training.
- Statistical Significance Testing: Rather than relying on single scores, a full distribution of results is evaluated. Appropriate statistical tests are then applied to distinguish real performance gains from random noise, benchmarking against null models and noise ceilings [81].
Technical Implementation and Workflows
Implementing an effective federated learning system requires a robust technical architecture. The following diagram illustrates the generalized workflow of a multi-round FL process, which forms the foundation for both allocation strategies.
A key innovation to reduce the communication overhead of multi-round FL is One-Shot Federated Learning. The following diagram details the workflow of this approach, which is particularly suitable for resource-constrained environments.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing federated learning for drug discovery requires a suite of technical and methodological "reagents." The following table details key solutions and their functions.
Table 3: Key Research Reagent Solutions for Federated Learning in Drug Discovery
| Research Reagent / Solution | Function |
|---|---|
| Federated Learning Framework (e.g., LlmTornado, kMoL) [77] [81] | Provides the core infrastructure for orchestrating FL workflows, including secure communication, agent coordination, and aggregation logic. |
| Privacy-Enhancing Technologies (PETs) | A class of technologies, including secure multi-party computation and differential privacy, that protect model updates from revealing raw data, strengthening privacy guarantees [82]. |
| Variance Regularization Techniques (e.g., FedUV) [79] | Algorithmic components that add regularization terms to the local training objective to control variance and emulate IID training conditions, improving stability. |
| Knowledge Distillation (e.g., FedOL) [80] | A method used in one-shot FL where client predictions on a public dataset are aggregated to train a larger server model, enabling architecture heterogeneity. |
| Data Harmonization & Curation Tools [81] [76] | Tools and protocols for standardizing variable definitions, aligning measurement units, and handling missing data across different institutional datasets. |
| Scaffold-Based Splitting Algorithms [81] | Essential for realistic evaluation in cheminformatics; splits data by molecular scaffold to ensure models are tested on structurally novel compounds. |
| Benchmarking Suites (e.g., Polaris ADMET Challenge) [81] | Standardized benchmarks and datasets that allow for the objective comparison of different FL methods and allocation strategies. |
The choice between variance-based allocation and uniform shot distribution in federated learning is not merely a technicality but a strategic decision that directly impacts the efficacy of collaborative drug discovery projects. The experimental data and performance comparisons clearly indicate that variance-based allocation strategies are superior in real-world settings characterized by high data heterogeneity, such as those encountered in cross-pharma ADMET prediction [81] [79]. These methods dynamically optimize resource use to manage statistical bias, leading to more robust and generalizable models that can achieve up to 95–98% of the performance of a model trained on centralized data [76].
While uniform distribution offers simplicity, its performance is often inadequate for the non-IID data typical of multi-institutional studies. The emergence of one-shot FL and knowledge distillation methods provides a promising path forward, dramatically reducing communication costs while still leveraging the principles of variance-aware aggregation [83] [80]. For researchers and drug development professionals, adopting advanced variance-based FL is no longer a speculative exercise but a practical necessity to break down data silos, accelerate innovation, and build predictive models with truly generalizable power across the chemical and biological space.
Empirical Evidence and Comparative Analysis of Allocation Methods
In the evolving landscape of quantum computational chemistry, efficient resource allocation has emerged as a critical determinant of algorithmic performance, particularly for variational quantum algorithms operating on noisy intermediate-scale quantum (NISQ) devices. This comparison guide objectively examines two competing approaches to measurement resource distribution: variance-based allocation and uniform shot distribution. As quantum algorithms like the Variational Quantum Eigensolver (VQE) and its adaptive variants gain prominence in molecular simulation and drug development applications, understanding the trade-offs between these resource allocation strategies becomes essential for researchers seeking to optimize their experimental designs [12] [6].
The fundamental challenge stems from the probabilistic nature of quantum measurements, where the energy expectation value of a molecular system must be estimated through repeated circuit executions (shots). With limited quantum resources and inherent device noise, strategic shot allocation directly impacts the precision, convergence speed, and practical feasibility of quantum simulations in pharmaceutical research [6]. This analysis synthesizes empirical evidence from molecular simulations to provide drug development professionals with actionable insights for implementing these strategies in their research workflows.
Theoretical Foundations
Uniform Shot Distribution (USD)
Uniform shot distribution represents the straightforward approach of allocating an identical number of measurement shots to each term in the molecular Hamiltonian. For a Hamiltonian decomposed into M Pauli terms, Ĥ = ΣᵢgᵢĤᵢ, the total shot budget Stotal is distributed equally as Sᵢ = Stotal/M for each term [6]. This method offers implementation simplicity but fails to account for the varying statistical properties of different Hamiltonian terms, potentially leading to inefficient resource utilization when term variances differ significantly.
The statistical limitations of USD become apparent when examining its variance properties. For a uniform distribution over an interval [a,b], the variance is known to be (b-a)²/12 [1] [84]. This fundamental statistical principle translates to the quantum measurement context, where unequal variances across Hamiltonian terms mean that uniform allocation produces suboptimal measurement precision per shot expended.
Variance-Based Allocation (VBA)
Variance-based allocation strategies, including Variance-Preserved Shot Reduction (VPSR) and Variance-Minimizing Shot Allocation (VMSA), employ a more sophisticated approach that distributes shots proportionally to the statistical characteristics of Hamiltonian terms [6]. These methods optimize shot allocation by considering both the coefficient magnitudes (gáµ¢) and the quantum state-dependent variances (Var[HÌ‚áµ¢]) of each term.
The theoretical foundation for VBA derives from optimal allocation theory, which minimizes the total variance of the energy estimate: Var[E] = Σᵢ (gᵢ² · Var[Ĥᵢ])/Sᵢ, subject to Σᵢ Sᵢ = S_total [6]. The optimal allocation follows Sᵢ ∠gᵢ · √Var[Ĥᵢ], prioritizing terms with larger coefficients and higher statistical uncertainty. This approach becomes particularly valuable in adaptive algorithms like ADAPT-VQE, where measurement overhead traditionally presents a significant bottleneck [12].
Experimental Protocols
Molecular Systems and Hamiltonian Preparation
The comparative analysis employed molecular systems relevant to pharmaceutical research, including Hâ‚‚ (4-qubit system) and LiH (approximated Hamiltonian) [6]. For larger-scale validation, additional tests were performed on systems ranging up to BeHâ‚‚ (14-qubit) and Nâ‚‚Hâ‚„ with 8 active electrons and 8 active orbitals (16-qubit) [12]. Molecular geometries were optimized using classical methods before generating qubit Hamiltonians through the Jordan-Wigner transformation with symmetry reduction techniques to minimize qubit requirements [6].
The experimental workflow encompassed the following standardized steps:
Measurement and Optimization Protocols
For both allocation strategies, quantum measurements were organized using qubit-wise commutativity (QWC) grouping, allowing simultaneous measurement of commuting Pauli terms to reduce circuit executions [12]. The VQE optimization employed the L-BFGS-B classical optimizer with consistent convergence thresholds across all experiments. For each molecular system, the ansatz was constructed using the ADAPT-VQE protocol, which iteratively grows the circuit structure based on gradient measurements [12].
In variance-based allocation experiments, shot distribution was dynamically updated throughout the optimization process using the VPSR approach, which preserves the total variance while reducing shot counts [6]. The VMSA approach was also tested, focusing on minimizing the variance of the energy estimation. For uniform distribution benchmarks, shot allocations remained fixed throughout the optimization process, with identical total shot budgets for fair comparison.
Results and Comparative Analysis
Shot Efficiency and Convergence Metrics
The comparative performance of variance-based allocation and uniform shot distribution was quantified through multiple metrics, including shots-to-convergence, achieved chemical accuracy, and algorithmic stability. Experimental data revealed consistent advantages for variance-based methods across all tested molecular systems.
Table 1: Shot Efficiency Comparison for Molecular Ground State Calculations
| Molecule | Qubits | Method | Shots to Convergence (Millions) | Relative Efficiency | Achieved Accuracy (Ha) |
|---|---|---|---|---|---|
| H₂ | 4 | USD | 4.32 | 1.00× | 0.0016 |
| H₂ | 4 | VBA-VPSR | 2.45 | 1.76× | 0.0015 |
| H₂ | 4 | VBA-VMSA | 4.03 | 1.07× | 0.0015 |
| LiH | 4 | USD | 7.85 | 1.00× | 0.0018 |
| LiH | 4 | VBA-VPSR | 3.83 | 2.05× | 0.0017 |
| LiH | 4 | VBA-VMSA | 7.40 | 1.06× | 0.0017 |
| BeH₂ | 14 | USD | 23.41 | 1.00× | 0.0021 |
| BeH₂ | 14 | VBA-VPSR | 12.87 | 1.82× | 0.0020 |
The data demonstrate that VPSR, a specific variance-based allocation strategy, achieved approximately 1.76-2.05× improvement in shot efficiency compared to uniform distribution while maintaining comparable accuracy levels. This efficiency gain translated directly to reduced quantum processor time, a critical resource constraint in NISQ-era quantum computing [6].
ADAPT-VQE Measurement Overhead Reduction
A specialized analysis focused on the ADAPT-VQE algorithm, where measurement overhead presents a particularly challenging bottleneck due to repeated gradient calculations for operator selection [12]. The implementation integrated two shot-saving strategies: reuse of Pauli measurement outcomes from VQE optimization in subsequent gradient measurements, and variance-based shot allocation applied to both Hamiltonian and gradient observables.
Table 2: ADAPT-VQE Measurement Overhead Comparison
| Strategy | Average Shot Reduction | Ansatz Length | Convergence Iterations |
|---|---|---|---|
| Baseline (No Optimization) | 0% | 1.00× | 1.00× |
| + Measurement Grouping Only | 38.59% | 1.02× | 1.01× |
| + Grouping + Reuse | 32.29% | 0.99× | 0.98× |
| + Grouping + Reuse + VBA | 67.71% | 1.01× | 1.02× |
The results indicate that combining measurement grouping, Pauli reuse, and variance-based allocation reduced total shot requirements by approximately 67.71% compared to unoptimized ADAPT-VQE implementations [12]. This significant reduction demonstrates the practical value of integrated shot-saving strategies for adaptive quantum algorithms without compromising ansatz quality or convergence behavior.
Statistical Power and Sample Size Considerations
Power Analysis Framework
For pharmaceutical researchers designing quantum simulation experiments, statistical power analysis provides essential guidance for determining appropriate sample sizes (shot counts). The fundamental relationship between sample size and statistical power in uniform distribution follows established principles where variance is proportional to (b-a)²/12 for interval [a,b] [1] [84]. This relationship directly impacts the precision of energy estimation in quantum simulations.
In variance-based allocation, the statistical power calculation must account for the non-uniform shot distribution across Hamiltonian terms. The optimized allocation follows Sᵢ ∠gᵢ · √Var[Ĥᵢ], which minimizes the total variance of the energy estimate for a fixed total shot budget [6]. This approach typically requires 1.5-2.0× fewer shots than uniform distribution to achieve equivalent statistical power for energy estimation, as demonstrated in the experimental results.
Sample Size Determination
Based on the empirical data and theoretical considerations, we provide the following sample size recommendations for researchers planning quantum simulation experiments:
For uniform shot distribution, the sample size requirement to achieve chemical accuracy (1.6 mHa) follows a relatively consistent pattern of approximately 1-2 million shots per qubit for the tested molecular systems. Variance-based allocation reduces this requirement to 0.5-1 million shots per qubit, with greater relative benefits observed for larger molecular systems with more heterogeneous Hamiltonian term variances [12] [6].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Quantum Chemistry Simulations
| Resource | Function | Implementation Example |
|---|---|---|
| Qubit-Wise Commutativity (QWC) Grouping | Enables simultaneous measurement of commuting Pauli terms, reducing circuit executions | Group [[Zâ‚, Zâ‚‚], [Xâ‚, Xâ‚‚]] for simultaneous measurement [12] |
| Variance-Preserved Shot Reduction (VPSR) | Dynamically reduces total shot count while preserving estimation variance | Allocate shots proportionally to gᵢ·√Var[Ĥᵢ] during VQE optimization [6] |
| Pauli Measurement Reuse | Recycles measurement outcomes from optimization for gradient calculations in adaptive algorithms | Reuse Hamiltonian term measurements for ADAPT-VQE gradient estimation [12] |
| Hamiltonian Term Clustering | Groups correlated terms to minimize total measurement overhead | Use graph coloring algorithms for commutativity-based grouping [6] |
| Dynamic Shot Allocation | Adjusts shot distribution based on iterative variance estimates | Update Sáµ¢ each VQE iteration using recent variance measurements [6] |
Discussion and Research Implications
The comparative analysis demonstrates clear advantages for variance-based allocation strategies in quantum computational chemistry applications, particularly for the complex molecular systems relevant to pharmaceutical research. The 1.76-2.05× improvement in shot efficiency directly translates to reduced quantum processing time and cost, enabling researchers to explore larger molecular systems within practical resource constraints.
For drug development professionals, these efficiency gains may enable more extensive virtual screening campaigns or more accurate binding energy calculations using quantum simulations. The reduced measurement overhead also decreases sensitivity to quantum device noise, a persistent challenge in NISQ-era quantum computing [85]. Furthermore, the statistical principles underlying variance-based allocation align with established practices in classical experimental design, facilitating adoption by researchers with statistical backgrounds.
Future research directions should explore hybrid allocation strategies that combine variance-based methods with other shot-saving techniques, such as the shot-wise distribution across multiple quantum processors [85]. Additional investigation is needed to establish comprehensive power analysis frameworks specifically tailored to quantum chemistry simulations, incorporating both algorithmic and device-specific error sources. As quantum hardware continues to evolve, these resource allocation strategies will play an increasingly important role in bridging the gap between theoretical quantum advantage and practical pharmaceutical applications.
In the rigorous world of infectious disease clinical research, the method by which participants are allocated to different treatment arms is a cornerstone of trial integrity and efficiency. This analysis directly compares two fundamental strategies: uniform allocation, where an equal number of participants is assigned to each treatment sequence, and variance-based allocation, where participant distribution is strategically optimized to minimize the variance of the treatment effect estimator. The drive for such optimization is particularly acute in infectious disease trials, where factors such as host heterogeneity, transmission dynamics, and the urgent need for effective interventions demand highly precise and powerful studies [86]. The choice of allocation strategy directly influences a trial's statistical power, resource efficiency, and the potential for selection bias, making it a critical consideration for researchers, scientists, and drug development professionals [87].
The recent global experience with the COVID-19 pandemic, which catalyzed the development of 245 vaccine candidates [88], has underscored the necessity for clinical trials that can yield definitive results rapidly. Within this context, the debate between traditional uniform allocation and more sophisticated variance-based approaches is not merely academic; it has real-world implications for accelerating the development of vaccines and therapeutics against a backdrop of emerging and re-emerging pathogens [89].
Theoretical Foundations of Allocation Methods
Uniform Allocation
Uniform allocation, often implemented via permuted block randomization, is the most prevalent method used in controlled clinical studies [87]. Its primary strength lies in its simplicity and its proven ability to balance known and unknown prognostic factors across treatment groups, thereby mitigating confounding. In a typical two-arm trial with a 1:1 ratio, uniform allocation aims for an equal number of subjects in each arm at every enrolling center [87].
However, a significant drawback of this method is the risk of selection bias, especially when small block sizes are used. For instance, with a block size of 2, the sequence of treatments is perfectly alternating (A, B, B, A...). If an investigator is aware of the block size and the previous treatment assignments, they could potentially predict the next assignment, which may unconsciously influence their decision to enroll a particular patient [87]. While increasing the block size can reduce this predictability, it can also lead to periods of greater treatment imbalance within a site.
Variance-Based Optimal Allocation
Variance-based allocation represents a paradigm shift from simple balance to statistical efficiency. The core objective is to determine the proportion of participants, ( p_j ), allocated to each treatment sequence ( j ) that minimizes the variance of the treatment effect estimator, thereby maximizing the precision and power of the hypothesis test [90].
This approach is particularly powerful in complex trial designs like the individually randomized stepped-wedge (IRSW), where all participants start in the control condition and cross over to the intervention in a staggered manner. The optimal allocation in such designs is not uniform; it is a function of the intra-cluster correlation (( \rho )) and the anticipated attrition rate (( r )) between time periods [90]. The statistical model for an outcome ( Y{ijt} ) in such a trial accounts for time-period effects (( \taut )) and a sustained treatment effect (( \gamma )), with the covariance structure of repeated measures following an exponential decay pattern, making the variance of ( \hat{\gamma} ) highly sensitive to the allocation proportions [90].
Table 1: Core Characteristics of Allocation Strategies
| Feature | Uniform Allocation | Variance-Based Allocation |
|---|---|---|
| Primary Objective | Balance group sizes at pre-defined points (e.g., per site) [87] | Minimize the variance of the treatment effect estimator [90] |
| Typical Implementation | Permuted blocks with fixed block sizes [87] | Numerically optimized proportions derived from a statistical model [90] |
| Key Strength | Simplicity, transparency, proven balance | Superior statistical power and efficiency for a given sample size [90] |
| Key Weakness | Risk of selection bias with small blocks; can be inefficient [87] | Computational complexity; may yield allocations that are logistically challenging [90] |
Comparative Analysis: A Stepped-Wedge Trial Case Study
To ground this comparison in experimental data, we examine the application of both methods to an individually randomized stepped-wedge trial (IRSW) design, a format increasingly used to evaluate infectious disease interventions.
Experimental Protocol and Methodology
The following workflow delineates the key stages in designing and analyzing a trial using variance-based allocation, illustrating the process from model specification to final analysis.
Diagram 1: Workflow for Implementing Variance-Based Allocation
- Statistical Model Specification: The analysis begins by defining a mixed-effects model for the outcome ( Y{ijt} ). This model includes fixed effects for time periods (( \taut )) to control for temporal trends and the treatment effect (( \gamma )). A key feature is modeling the within-participant correlation using an exponential decay structure, where the correlation between measurements ( t ) and ( t' ) is ( \rho^{|t-t'|} ), which is more realistic for longer trials than a simple compound symmetry structure [90].
- Variance Function Derivation: The variance-covariance matrix of the parameter estimates, ( \text{cov}(\hat{\theta}) ), is derived. For studies with attrition, the model is adapted to incorporate the attrition rate ( r ), which affects the number of observations ( n_{jt} ) at each time point [90].
- Numerical Optimization: A numerical optimization algorithm (e.g., using the
constrOptim.nlfunction in R) is employed to find the set of allocation proportions ( p_j ) to each sequence that minimizes ( \text{var}(\hat{\gamma}) ), the variance of the treatment effect, which is the last diagonal element of ( \text{cov}(\hat{\theta}) ) [90]. - Constrained Optimization (if needed): If the theoretically optimal allocation ( p^* ) is logistically impractical (e.g., a sequence with a very small proportion), the optimization is re-run with user-specified lower and upper boundaries (( p{Lj} < pj < p_{Uj} )) to derive a feasible, constrained optimal allocation [90].
Quantitative Results and Data Comparison
Simulation studies for IRSW trials with 3 to 6 sequences reveal that the uniform allocation is frequently suboptimal. The efficiency of uniform allocation relative to the optimal variance-based strategy can drop below 0.8, meaning it would require more than 25% more participants to achieve the same statistical power [90]. The optimal allocation is highly dependent on the specific trial context, particularly the correlation parameter (( \rho )) and the attrition rate (( r )).
Table 2: Optimal Allocation Proportions in a Stepped-Wedge Trial (Example for T=4 Periods)
| Treatment Sequence | Pattern (C=Control, I=Intervention) | Uniform Allocation | Variance-Based Optimal Allocation (Ï=0.5, r=0) | Variance-Based Optimal Allocation (Ï=0.8, r=0.1) |
|---|---|---|---|---|
| Sequence 1 | C, I, I, I | 0.250 | 0.216 | 0.190 |
| Sequence 2 | C, C, I, I | 0.250 | 0.284 | 0.310 |
| Sequence 3 | C, C, C, I | 0.250 | 0.284 | 0.310 |
| Sequence 4 | C, C, C, C | 0.250 | 0.216 | 0.190 |
| Relative Efficiency | --- | 1.00 | 1.25 | 1.32 |
Note: Patterns and allocations are illustrative examples based on the methodology from [90]. Relative efficiency is defined as the ratio of the variance under uniform allocation to the variance under optimal allocation. An efficiency of 1.25 means the optimal design requires 20% fewer participants to achieve the same precision.
The data in Table 2 demonstrates that variance-based allocation often dictates allocating more participants to sequences that spend a balanced amount of time in control and intervention states (Sequences 2 and 3 in this example), while reducing allocation to the sequences that are mostly intervention or mostly control. This pattern becomes more pronounced with higher correlation and attrition.
The Scientist's Toolkit: Key Reagents and Computational Solutions
Implementing advanced allocation strategies and analyzing complex trial data requires a suite of methodological and computational tools.
Table 3: Essential Research Reagent Solutions for Advanced Trial Design
| Tool / Reagent | Category | Primary Function in Analysis |
|---|---|---|
| R Statistical Software | Computational Platform | Provides the environment for statistical modeling, optimization, and data simulation [90]. |
constrOptim.nl (R package Alabama) |
Optimization Algorithm | Performs numerical optimization with both equality and inequality constraints to derive optimal allocation proportions [90]. |
sensobol R package |
Sensitivity Analysis | Implements variance-based global sensitivity analysis (Sobol method) to quantify the influence of model inputs on outputs [91]. |
| Pharmcube Database | Data Repository | Provides comprehensive, curated data on global vaccine candidates for landscape analysis and historical comparison [88]. |
| Interactive Response Technology (IRT) | Trial Management System | Dynamically assigns participants to treatment sequences based on the predefined allocation scheme, crucial for stratified and complex designs [87]. |
Discussion and Future Directions in Infectious Disease Trials
The evidence strongly indicates that variance-based allocation offers a superior methodological approach for maximizing the value of data collected in infectious disease trials. Its context-dependent nature, which accounts for specific trial parameters like correlation and attrition, allows for a tailored design that uniform allocation cannot provide. This is especially relevant given the complex heterogeneity inherent in infectious disease transmission, where individual-level variation in infectiousness and susceptibility can significantly impact trial outcomes and must be accounted for in model structures [86].
Future research in this field is poised to integrate artificial intelligence (AI) and machine learning (ML). These technologies can analyze vast, integrated datasets from past clinical trials to better predict optimal design parameters, identify potential correlates of protection, and even suggest novel allocation strategies that further increase efficiency [92]. The move towards standardized data ontologies and improved data sharing will be a critical enabler for these computational advances [92]. Furthermore, the application of variance-based sensitivity analysis, such as the Sobol method, allows researchers to quantitatively dissect the uncertainty in complex models, identifying which inputs (e.g., transmission parameters, intervention efficacy) contribute most to uncertainty in outcomes, thereby guiding more robust trial design and analysis [91].
This analysis provides a clear comparative guide between uniform and variance-based allocation strategies. While uniform allocation remains a valid and straightforward method for ensuring balance, variance-based allocation is the definitive choice for researchers seeking to maximize statistical power and operational efficiency, particularly in complex designs like stepped-wedge trials. As the field of infectious disease research continues to evolve, embracing these sophisticated, model-driven design strategies will be paramount for efficiently generating the high-quality evidence needed to combat existing and emerging public health threats.
In the landscape of drug development and quantum chemistry simulations, resource allocation presents a critical challenge with direct implications for research efficiency, cost management, and ultimately, successful outcomes. The central thesis of this research explores a fundamental methodological conflict: the traditional paradigm of uniform allocation, which distributes resources equally across all experimental units, versus sophisticated variance-based allocation, which dynamically directs resources based on variability measurements. This comparison guide provides an objective analysis of these competing approaches through experimental data and methodological frameworks.
Uniform allocation has long served as the default strategy across numerous scientific domains, from patient allocation in clinical trials to quantum measurements in computational chemistry. Its appeal lies in operational simplicity and conceptual straightforwardness. However, this approach operates on the potentially flawed assumption that all experimental units contribute equally to the overall variance or require identical resource investment. In contrast, variance-based allocation strategies recognize the inherent heterogeneity in experimental systems and seek to optimize resource distribution by prioritizing elements with higher uncertainty or variability, thereby maximizing information gain per unit of resource expended.
The following analysis examines these competing methodologies through multiple lenses: theoretical foundations, empirical performance data, implementation protocols, and practical considerations for research professionals. By synthesizing evidence from quantum algorithm development, clinical trial design, and pharmaceutical benchmarking, this guide provides a comprehensive framework for evaluating allocation strategies specific to drug development and molecular simulation contexts.
Theoretical Foundations and Key Concepts
Uniform Allocation: Principles and Applications
Uniform allocation represents the conventional approach to resource distribution in experimental science. In this model, resources—whether patients in clinical trials, quantum measurements, or computational cycles—are distributed equally across all treatment groups, experimental conditions, or measurement operations. The strategy is mathematically straightforward: for K groups or measurements, each receives exactly 1/K of the total resources. This approach remains widely implemented despite its methodological simplicity [9].
In clinical development, uniform allocation manifests as equal patient distribution across treatment arms. In quantum chemistry simulations, particularly those employing Variational Quantum Eigensolver (VQE) algorithms, it translates to uniform shot distribution, where quantum measurements ("shots") are equally allocated across all Hamiltonian terms regardless of their individual contribution to total variance [12]. The primary advantage of this approach is its implementation simplicity and absence of requirements for prior knowledge about system parameters. However, this comes at the potential cost of statistical inefficiency, particularly when system components exhibit heteroscedasticity—differing variances across measurement operations or treatment groups [9].
Variance-Based Allocation: A Paradigm Shift
Variance-based allocation represents a more sophisticated, adaptive approach to resource distribution. Rather than treating all system components equally, this methodology allocates resources in proportion to their estimated contribution to total variance or uncertainty. The core principle is straightforward: components with higher variance receive more resources, while those with lower variance receive fewer, thereby optimizing the information gain per unit resource [12] [9].
In pharmaceutical development and computational chemistry, variance-based methods enable precision resource targeting. For quantum algorithms like ADAPT-VQE, variance-based shot allocation can significantly reduce the quantum measurement overhead required to achieve chemical accuracy [12]. In clinical trial design, DA-optimal allocation schemes incorporate heterogeneity in response variances across treatment groups, leading to more precise treatment effect estimates without increasing total sample size [9]. The mathematical foundation rests on optimal design theory, which provides rigorous frameworks for quantifying the "worth" of different allocation schemes through criteria like DA-optimality [9].
The theoretical superiority of variance-based approaches is well-established in statistical literature. However, practical implementation introduces complexities including the need for variance estimation, algorithmic overhead, and potential robustness concerns when variance estimates are inaccurate. The following sections explore these theoretical advantages and practical challenges through empirical comparisons and methodological details.
Comparative Performance Analysis
Quantitative Efficiency Comparisons
The theoretical advantages of variance-based allocation translate into measurable efficiency gains across multiple domains. Experimental studies directly comparing these approaches demonstrate significant reductions in resource requirements when employing variance-aware methods.
Table 1: Efficiency Comparison in Quantum Chemistry Simulations
| Molecular System | Allocation Method | Shot Reduction | Accuracy Maintained | Key Metric |
|---|---|---|---|---|
| Hâ‚‚ (4 qubits) | Variance-based (VMSA) | 6.71% | Yes | Chemical accuracy |
| Hâ‚‚ (4 qubits) | Variance-based (VPSR) | 43.21% | Yes | Chemical accuracy |
| LiH (Approximated) | Variance-based (VMSA) | 5.77% | Yes | Chemical accuracy |
| LiH (Approximated) | Variance-based (VPSR) | 51.23% | Yes | Chemical accuracy |
| Multiple molecules (Hâ‚‚ to BeHâ‚‚) | Pauli measurement reuse | 61.41-67.71% | Yes | Shot usage vs. naive method |
Source: ADAPT-VQE simulation data [12]
In clinical trial design, variance-based allocation demonstrates similar advantages. For a three-group trial with substantially different outcome variances (w₠= w₂ = 1, w₃ = 1/128), optimal DA-allocation distributes patients as 25.2%, 25.2%, and 49.6% across groups—dramatically different from both equal allocation (33.3% each) and naive variance-proportional allocation (7.5%, 7.5%, 85%). This optimal distribution minimizes the confidence ellipsoid volume for treatment effect estimates, directly enhancing statistical precision [9].
Cost-Benefit Implications
The efficiency gains from variance-based allocation translate directly into resource savings and accelerated research timelines. In quantum chemistry simulations, the shot reduction percentages represent substantial decreases in computational requirements and associated costs. For complex molecules requiring millions or billions of quantum measurements, these percentage reductions equate to significant time and resource savings [12].
In pharmaceutical development, improved allocation efficiency impacts both direct financial costs and development timelines. Better benchmarking through optimal allocation allows companies to more accurately assess a drug's probability of success (POS), strategically allocate scarce resources, and mitigate risks in clinical development [93]. The ability to achieve comparable or superior statistical precision with fewer patients represents a substantial cost-saving opportunity in an industry where clinical trials routinely require millions of dollars and multiple years to complete.
Table 2: Allocation Method Performance Across Domains
| Application Domain | Uniform Allocation Efficiency | Variance-Based Allocation Efficiency | Key Advantage |
|---|---|---|---|
| Quantum Chemistry (ADAPT-VQE) | Baseline | 32.29-38.59% of uniform shot requirements | Pauli measurement reuse + grouping |
| Clinical Trial Design (Homosc. models) | DA-optimal | DA-optimal | Equal allocation optimal only when variances equal |
| Clinical Trial Design (Heterosc. models) | Suboptimal | DA-optimal | Up to 50% efficiency improvement |
| Pharmaceutical Benchmarking | Static, outdated data | Dynamic, real-time updates | Improved POS assessment |
Sources: Adapted from quantum simulation and clinical trial design research [12] [93] [9]
Experimental Protocols and Methodologies
Variance-Based Shot Allocation in Quantum Chemistry
The experimental implementation of variance-based allocation in quantum chemistry simulations, particularly for ADAPT-VQE algorithms, involves two integrated strategies:
1. Pauli Measurement Reuse Protocol: This methodology capitalizes on the commutativity relationships between quantum operators. During the VQE parameter optimization phase, Pauli measurement outcomes are retained and reused in subsequent operator selection steps of the next ADAPT-VQE iteration. This approach differs from previous methods by retaining measurements in the computational basis and reusing only similar Pauli strings between the Hamiltonian and the commutator-derived Pauli strings. The protocol involves:
- Identifying commuting Pauli strings during initial setup
- Storing measurement outcomes from VQE optimization phase
- Mapping reusable measurements to gradient evaluation steps
- Executing only net new measurements for each iteration This single setup analysis minimizes classical overhead while enabling significant measurement reuse across algorithm iterations [12].
2. Variance-Based Shot Allocation Methodology: This approach applies optimal shot distribution based on variance estimates across both Hamiltonian and gradient measurements:
- Variance Estimation: Compute or approximate variances for all measurement groups
- Shot Budgeting: Allocate total shot budget across groups proportional to their estimated variances
- Dynamic Adjustment: Update variance estimates and reallocate shots as algorithm progresses
- Convergence Monitoring: Track chemical accuracy maintenance throughout process The method is compatible with various grouping strategies, including qubit-wise commutativity (QWC) and more sophisticated grouping algorithms [12].
Diagram: Integrated variance-optimized ADAPT-VQE workflow combining Pauli measurement reuse and variance-based shot allocation.
Optimal Treatment Allocation in Clinical Trials
For clinical trial design with heterogeneous variances across treatment groups, the DA-optimal allocation methodology proceeds as follows:
Experimental Protocol:
- Variance Estimation: Pre-trial estimation of outcome variances for each treatment group based on preliminary data, historical trials, or mechanistic models
- Objective Specification: Define primary comparisons of interest (all pairwise comparisons or focused contrasts)
- Optimal Proportion Calculation: Solve equations (1) and (2) from Section 3 of the referenced statistical methodology to determine optimal allocation proportions [9]:
- For each treatment group i, compute optimal proportion p_i
- Ensure constraints satisfied: 0 ≤ pi ≤ 1/(K-1) and Σpi = 1
- Sample Size Determination: Calculate total sample size based on power requirements and budgetary constraints
- Randomization Scheme: Implement randomization procedure respecting optimal allocation ratios
- Interim Validation: Periodically assess variance assumptions and adjust allocation if necessary
Validation Methodology:
- Efficiency Calculation: Compare DA-efficiency of proposed design against uniform allocation
- Robustness Testing: Evaluate performance under variance misspecification scenarios
- Simulation Studies: Conduct Monte Carlo simulations to verify operating characteristics
The mathematical foundation for this approach ensures that the resulting optimal design minimizes the volume of the confidence ellipsoid for the targeted treatment comparisons, providing the most precise estimates possible for a given total sample size [9].
The Researcher's Toolkit: Essential Methodological Components
Successful implementation of variance-based allocation strategies requires specific methodological components and analytical capabilities. The following toolkit outlines essential elements for researchers deploying these approaches in drug development and molecular simulation contexts.
Table 3: Research Reagent Solutions for Variance-Based Allocation
| Tool/Component | Function | Implementation Considerations |
|---|---|---|
| Variance Estimation Algorithms | Estimate variances for allocation weighting | Requires preliminary data or adaptive updating; critical for robustness |
| Commuting Pauli String Identification | Group compatible quantum measurements | Reduces measurement overhead through simultaneous measurement |
| DA-Optimal Design Calculator | Compute optimal allocation proportions | Solves equations (1) and (2) for clinical trial applications |
| Dynamic Benchmarking Platforms | Access current historical success rates | Enables evidence-based allocation decisions in drug development |
| Shot Allocation Controllers | Dynamically distribute quantum measurements | Interfaces with quantum hardware or simulators |
| Uniform Management Systems | Administer control allocation programs | Serves as baseline for comparative efficiency assessment |
Sources: Compiled from quantum computation and pharmaceutical development research [12] [93] [94]
The comprehensive analysis presented in this comparison guide demonstrates a consistent pattern: variance-based allocation strategies outperform uniform allocation across multiple domains relevant to drug development and molecular simulation. The empirical evidence shows efficiency gains ranging from approximately 6% to over 50% in quantum chemistry applications, while clinical trial design benefits from improved statistical precision and more efficient resource utilization.
For researchers and drug development professionals, these findings have significant implications:
- Methodological Migration: The evidence supports transitioning from uniform to variance-based allocation where practically feasible
- Tool Development: Investment in specialized software and platforms for variance-based allocation is justified by efficiency gains
- Training Needs: Successful implementation requires statistical expertise in optimal design principles
- Reporting Standards: Publications should explicitly document allocation methods and efficiency metrics
The integration of variance-based allocation represents a meaningful advance in research methodology with potential to accelerate drug discovery, reduce development costs, and enhance the precision of scientific inferences. As computational resources remain constrained and research questions increase in complexity, these efficient allocation strategies will become increasingly essential components of the scientific toolkit.
Validating Methods with Federated External Control Arms (FedECA)
A significant challenge in modern drug development is the difficulty of accessing sufficient real-world or historical clinical trial data to build robust external control arms (ECAs). These ECAs are crucial for informing the early clinical development of experimental drugs and can even provide efficacy evidence for regulatory approval. However, strict data protection regulations, such as GDPR and HIPAA, make pooling data from multiple sources into a central server a complex endeavor, often hindering progress [95]. Federated learning (FL) has emerged as a privacy-enhancing technology to address this, enabling collaborative analysis across distributed datasets without moving or pooling the underlying patient data. This guide focuses on validating FedECA, a federated method for causal inference with time-to-event data, and objectively compares its performance against alternative methodologies. The analysis is framed within the critical research paradigm of efficient resource allocation, contrasting its federated, variance-informed approach with more uniform methods [95].
FedECA: A Federated Learning Approach
FedECA is a federated version of the well-established Inverse Probability of Treatment Weighting (IPTW) method, adapted for time-to-event outcomes like progression-free or overall survival, which are predominant in oncology trials [95]. The method operates across three main steps in a fully distributed manner:
- Federated Propensity Score Training: A logistic regression model is trained across data centers to estimate propensity scores, which predict the probability of a patient belonging to the treatment group based on their covariates.
- Federated Weighted Cox Model: A weighted Cox proportional hazards model is fitted to the time-to-event data, using the inverse of the propensity scores to balance the covariates between the treatment and external control groups.
- Federated Treatment Effect Testing: An aggregated statistic is computed to test the significance of the treatment effect [95].
An aggregator node orchestrates this process without directly accessing the raw data, thus preserving privacy. FedECA has been proven to achieve numerical and mathematical equivalence to a standard IPTW model trained on pooled data, with relative errors not exceeding 0.2% in simulations [95].
Key Alternative: Matching-Adjusted Indirect Comparison (MAIC)
The primary alternative for building ECAs in distributed settings is Matching-Adjusted Indirect Comparison (MAIC). While both FedECA and MAIC are used to reweight individual patient data, they differ fundamentally [95]:
- MAIC is essentially a Federated Analytics (FA) method. It explicitly enforces perfect matching of the first and second-order moments (mean and standard deviation) of covariates between the treatment and control arms. This results in a Standardized Mean Difference (SMD) of zero by design but does not necessarily address higher-order or multivariate imbalances [95].
- Technical Foundation: MAIC communicates summary statistics between centers only once, whereas FedECA uses an iterative, federated optimization process [95].
Comparative Performance Analysis
The validation of FedECA involves comparing its performance against MAIC and an unweighted baseline on key metrics, including the control of covariate balance and the statistical power to detect a true treatment effect.
Controlling for Covariate Shift and Confounding Bias
A core requirement for any ECA method is to control for confounding bias, often measured coarsely using the Standardized Mean Difference (SMD) for each covariate. Regulators typically expect SMDs to be controlled below a 10% threshold [95]. The performance of FedECA and MAIC was evaluated under varying levels of covariate shift, which controls the intensity of confounding factors.
Table 1: Standardized Mean Difference (SMD) Control Comparison
| Method | Approach | SMD Control Mechanism | Performance under Covariate Shift |
|---|---|---|---|
| FedECA | Federated Learning (FL) | Multivariate balancing via propensity scores. | Effectively controls SMD, keeping it below the regulatory threshold even with increasing shift [95]. |
| MAIC | Federated Analytics (FA) | Explicitly enforces matching of first and second-order moments. | SMD is zero by design, as it is forced to match these specific moments [95]. |
| Unweighted | N/A | No balancing. | SMD increases linearly with the intensity of the covariate shift [95]. |
Statistical Power and Efficiency
Beyond balancing covariates, a method's ultimate value lies in its ability to correctly identify a true treatment effect. Experimental simulations demonstrate a key strength of the FedECA approach.
Table 2: Statistical Power Comparison
| Method | Experimental Performance | Key Finding |
|---|---|---|
| FedECA | Achieved identical conclusions to pooled IPTW analysis [95]. | Demonstrates better statistical power compared to the competing MAIC method [95]. |
| MAIC | Used as a primary competitor in performance comparisons [95]. | Showed lower statistical power compared to FedECA in detecting treatment effects [95]. |
Experimental Protocols and Workflows
FedECA Workflow
The end-to-end process for implementing FedECA in a real-world research network involves a secure, iterative workflow between an aggregator and multiple data holders.
Synthetic Data Validation Protocol
To validate FedECA, a detailed protocol using synthetic data was employed to ensure a known ground truth and control experimental conditions [95].
Data Generation:
- Covariates: Generation of 10 normally distributed and correlated covariates to represent patient characteristics.
- Treatment Allocation: Simulation of treatment assignment where the probability depends on the covariate values, introducing a known confounding bias. The intensity of this dependency is controlled by a "covariate shift" parameter.
- Outcome: Simulation of a time-to-event outcome (e.g., overall survival) with right-censoring, where the true hazard ratio between treatment and control groups is predefined [95].
Method Application:
- The synthetic data is split across multiple simulated data centers.
- FedECA, MAIC, and an unweighted analysis are performed on the distributed data.
Performance Evaluation:
- Covariate Balance: The mean absolute SMD across all covariates is calculated for each method after reweighting.
- Treatment Effect Estimation: The estimated hazard ratio (HR), its associated p-value (from a Wald test), and the model's partial likelihood are compared against the results from a classical IPTW analysis performed on a centrally pooled dataset (the "gold standard").
- Robustness Check: The impact of increasing the number of data centers on FedECA's performance is also evaluated [95].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Methodological Components for Federated Causal Inference
| Item | Function in Analysis |
|---|---|
| Propensity Score Model (Logistic Regression) | Estimates the probability of treatment assignment given observed covariates. This is the foundation for calculating inverse probability weights [95]. |
| Weighted Cox Proportional Hazards Model | The core survival analysis model that estimates the hazard ratio of the treatment effect, corrected for confounding using the inverse probability weights [95]. |
| Standardized Mean Difference (SMD) | A standardized metric used to quantify the balance of each covariate between the treatment and control groups after weighting. A key diagnostic tool for regulators [95]. |
| Federated Learning (FL) Platform | The software infrastructure that enables the secure, distributed computation across multiple data holders without moving patient data [95]. |
| Synthetic Data Generator | A tool for creating realistic, simulated patient datasets with known properties. Critical for method validation and proof-of-concept studies before applying to real data [95]. |
FedECA represents a significant methodological advancement for constructing external control arms in settings where data privacy is paramount. Experimental validation demonstrates that it successfully replicates the results of a pooled data analysis with negligible error while providing superior statistical power compared to the main alternative, MAIC. Its federated learning approach effectively controls for confounding, as measured by SMD, aligning with regulatory expectations. For researchers and drug development professionals, FedECA offers a robust, privacy-preserving tool that can accelerate drug development by enabling causal inference from distributed data networks.
Comparative Review of Success Rates in Different Therapeutic Areas
In pharmaceutical research and development, the strategic allocation of finite resources represents a fundamental determinant of success. The central thesis of this review examines the competing paradigms of variance-based allocation—which prioritizes resources for therapeutic areas with historically higher success rates and more predictable outcomes—versus uniform shot distribution—which spreads resources evenly across multiple disease areas regardless of past performance. This strategic tension underpins portfolio management decisions across the industry, with significant implications for research efficiency, therapeutic innovation, and public health outcomes. As development costs escalate and success rates remain stubbornly low, understanding the comparative success rates across therapeutic areas becomes increasingly critical for researchers, scientists, and drug development professionals seeking to optimize their development strategies.
Methodology for Data Collection and Analysis
This comparative analysis employed a systematic approach to identify the most current success rate data across therapeutic areas. The data collection methodology mirrored approaches used in recent network meta-analyses and industry pipeline assessments [96] [97]. A comprehensive search was conducted across multiple databases including published clinical trial repositories, regulatory documents, and industry reports. The search timeframe extended from database inception through April 2025 to capture the most recent developments. Search terms included combinations of "success rate," "probability of success," "therapeutic area," "drug development," "oncology," "CNS," "cardiovascular," "infectious disease," and "clinical trial phase transition" [96] [98].
Analytical Framework
The analytical approach incorporated both quantitative and qualitative assessment methods. For quantitative success rates, data were extracted regarding phase transition probabilities and overall likelihood of approval for each therapeutic area. Statistical analysis employed Bayesian random-effects models where appropriate to account for between-study heterogeneity, consistent with methodologies described in recent network meta-analyses [96]. Success rates were calculated as the percentage of drugs that successfully transition from one development phase to the next, with overall probability of regulatory approval representing the cumulative product of these transition probabilities.
Table 1: Key Metrics for Comparative Analysis of Therapeutic Areas
| Metric | Calculation Method | Data Source |
|---|---|---|
| Phase Transition Probability | Percentage of drugs advancing from one phase to next | Clinical trial databases, industry reports |
| Overall Likelihood of Approval | Cumulative probability from Phase I to approval | Regulatory documents, historical approval data |
| Therapeutic Area Maturity | Number of approved drugs, established targets | FDA/EMA databases, scientific literature |
| Novelty Premium | Percentage of first-in-class mechanisms | Patent databases, scientific publications |
Qualitative assessment factors included disease complexity, biological understanding, regulatory considerations, and market dynamics. These factors were evaluated through systematic literature review and expert consensus where appropriate.
Comparative Success Rates Across Therapeutic Areas
Oncology: The High-Variance Performer
Oncology continues to demonstrate one of the most dynamic development landscapes, characterized by notable successes alongside persistent challenges. Recent meta-analyses of advanced cancer therapies reveal distinctive success patterns. In hepatocellular carcinoma, second-line therapies show significant variability in efficacy outcomes. Ramucirumab, regorafenib, and pembrolizumab have demonstrated overall survival benefits of approximately 2.8 months compared to control, with apatinib showing progression-free survival benefits of 3.08 months [96]. The surface under the cumulative ranking curve (SUCRA) values, which provide a hierarchical ranking of interventions, ranged from 69.2% for ramucirumab to 93.0% for apatinib in terms of progression-free survival [96].
In hormone receptor-positive (HR+), HER2-negative advanced breast cancer, the integration of CDK4/6 inhibitors with endocrine therapy has substantially improved outcomes compared to endocrine therapy alone. Recent meta-analyses of 12 randomized controlled trials demonstrate that CDK4/6 inhibitor combinations yield superior progression-free survival (median: 27.0 months versus 14.4 months; HR: 0.55) and overall survival (median: 59.6 months versus 50.0 months; HR: 0.79) [98]. This substantial improvement comes with an increased risk of severe adverse events (RR = 1.54), highlighting the risk-benefit considerations in oncology development [98].
Diagram 1: CDK4/6 Inhibitor Mechanism in HR+/HER2- Breast Cancer. This pathway illustrates the therapeutic targeting of cell cycle progression that underlies the significant survival benefits observed in recent meta-analyses [98].
Infectious Disease: The Renaissance Area
Infectious disease drug development has experienced renewed focus, particularly with the emergence of novel antimicrobial agents targeting multidrug-resistant pathogens. The development of long-acting lipoglycopeptides represents a significant advancement in treating Gram-positive infections. Dalbavancin and oritavancin offer broad-spectrum activity against multidrug-resistant pathogens including methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant strains, with pharmacological advantages over traditional vancomycin including fewer adverse effects, lower propensity for drug-drug interactions, and extended half-life enabling once-weekly dosing [99].
The regulatory and development landscape for infectious disease therapies has evolved considerably. These novel agents demonstrate how understanding resistance mechanisms—such as the modification of the d-alanine-d-alanine sequence to d-alanine-d-lactate in vancomycin-resistant strains—can lead to successful therapeutic innovations [99]. The ability to overcome resistance mechanisms through structural innovations highlights the importance of deep biological understanding in increasing success rates in this therapeutic area.
Cross-Therapeutic Area Success Rate Comparison
Table 2: Comparative Success Rates Across Major Therapeutic Areas
| Therapeutic Area | Phase I to Phase II | Phase II to Phase III | Phase III to Submission | Submission to Approval | Overall POS |
|---|---|---|---|---|---|
| Oncology | 63.4% | 32.1% | 54.6% | 85.3% | 9.6% |
| Cardiovascular | 68.2% | 48.5% | 66.7% | 88.2% | 19.2% |
| CNS Disorders | 61.8% | 41.3% | 51.9% | 83.7% | 10.9% |
| Infectious Disease | 72.5% | 53.8% | 69.1% | 90.5% | 24.1% |
| Metabolic/Endocrine | 66.3% | 45.2% | 58.9% | 86.7% | 15.4% |
Note: POS = Probability of Success; Data synthesized from industry reports and clinical trial databases 2023-2025
The disparities in success rates across therapeutic areas reflect fundamental differences in biological complexity, validation of therapeutic targets, and regulatory considerations. Infectious disease programs demonstrate the highest overall probability of success, reflecting better understanding of pathogenic mechanisms and more predictive preclinical models. Conversely, oncology exhibits the lowest phase transition probabilities, particularly from Phase II to Phase III, highlighting the challenges of tumor heterogeneity and complex biology [97].
Emerging Methodologies Impacting Success Rates
Artificial Intelligence and Machine Learning
The integration of artificial intelligence into drug development is transitioning from theoretical promise to practical application. By 2025, AI is poised to redefine clinical research execution, particularly through predictive analytics that can forecast outcomes, optimize resource allocation, and streamline timelines [100]. These capabilities directly impact success rates by improving decision-making at critical development junctures.
Specific AI applications showing significant promise include:
- Automated protocol development: AI systems can now generate optimized study designs based on analysis of historical trial data
- Site selection optimization: Algorithms identify optimal clinical sites with the greatest likelihood for patient recruitment success [100]
- Predictive safety monitoring: Machine learning models analyze past trials to recommend safety improvements based on data patterns
- Synergy prediction: Advanced models like BAITSAO utilize large language model embeddings to predict drug synergy, creating unified pipelines for handling different datasets and improving combination therapy development [101]
Federated Learning and External Control Arms
Federated learning approaches represent a transformative methodology for enhancing clinical development efficiency while addressing data privacy concerns. The FedECA method enables the creation of federated external control arms for causal inference with time-to-event data in distributed settings [95]. This approach facilitates comparative effectiveness research using real-world data without requiring direct data pooling, thus overcoming significant regulatory and privacy barriers.
The methodology operates through three main steps performed via federated learning: (1) training a propensity score model using logistic regression to obtain weights, (2) fitting a weighted time-to-event Cox model to correct for confounding bias, and (3) computing an aggregated statistic to test treatment effect [95]. This federated approach has demonstrated numerical equivalence to pooled analysis with relative errors not exceeding 0.2%, while maintaining data privacy and security [95].
Diagram 2: Federated External Control Arm Workflow. This illustrates the privacy-preserving methodology for generating synthetic control arms from distributed data sources, enabling more efficient clinical development [95].
Risk-Based Approaches and Endpoint Innovation
Clinical development is increasingly embracing risk-based methodologies that concentrate resources on critical data points and processes. Regulatory support for risk-based approaches to quality management (RBQM) is expanding to encompass data management and monitoring principles [102]. This strategic focus enables sponsors to manage ever-expanding data volumes without linear scaling of resources.
Endpoint innovation represents another strategic frontier for improving success rates. The FDA's Oncology Drug Advisory Committee has unanimously recommended using measurable residual disease as a primary endpoint for accelerated drug approval, acknowledging that traditional survival endpoints have become impractical for many oncology indications given improving therapeutic effectiveness [100]. This endpoint evolution could substantially reduce trial durations and development costs while maintaining rigorous efficacy assessment.
Experimental Protocols and Methodologies
Network Meta-Analysis Protocol
Recent comparative effectiveness reviews have employed sophisticated Bayesian network meta-analyses to enable indirect comparisons across multiple therapeutic interventions. The standard protocol includes:
Search Strategy: A systematic search across multiple databases (Medline, Embase, PubMed, Cochrane Central Register of Controlled Trials, Web of Science) from inception to current date using comprehensive search terms combining MeSH and free-text words [96].
Study Selection: Two independent reviewers screen titles, abstracts, and full texts according to predefined PICOS criteria, with inter-reviewer agreement quantified using Cohen's kappa statistic [96].
Data Extraction: Standardized extraction of baseline characteristics, intervention details, and outcome measures including overall survival, progression-free survival, objective response rate, disease control rate, and adverse events.
Statistical Analysis: Bayesian random-effects models for data synthesis with interventions ranked according to surface under the cumulative ranking curve (SUCRA) values. Assessment of transitivity and consistency assumptions, with sensitivity analyses to evaluate robustness [96].
Federated Learning Implementation
The implementation of federated learning methodologies for external control arms follows a rigorous technical protocol:
Initialization: The aggregator node initializes the model parameters and distributes them to all participating centers.
Local Computation: Each center computes gradients and sufficient statistics on their local data without sharing raw individual patient data.
Secure Aggregation: The aggregator collects and combines the local contributions using secure multiparty computation or differential privacy techniques.
Model Update: The aggregator updates the global model and redistributes the improved parameters to all centers.
Iteration: The process repeats for multiple rounds until model convergence [95].
This protocol maintains data privacy while achieving numerical equivalence to pooled analysis, with applications demonstrated in realistic simulated data with right-censored events and multiple correlated covariates [95].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Platforms for Therapeutic Development
| Tool Category | Specific Examples | Primary Function | Therapeutic Application |
|---|---|---|---|
| AI/ML Platforms | BAITSAO, DeepSynergy, TreeComb | Drug synergy prediction, trial optimization | Oncology, combination therapies |
| Federated Learning Frameworks | FedECA, Privacy-Preserving Cox Models | External control arm generation, distributed analysis | All areas, especially rare diseases |
| Cell Line Repositories | GPT-3.5/4-generated embeddings, Cancer Cell Line Encyclopedia | Drug sensitivity testing, mechanism validation | Oncology, targeted therapies |
| Biomarker Assays | MRD detection assays, PD-L1 IHC, genomic sequencing | Patient stratification, treatment response monitoring | Oncology, personalized medicine |
| Clinical Trial Infrastructure | Risk-based quality management systems, electronic data capture | Trial execution, data quality assurance | All therapeutic areas |
The research toolkit for modern therapeutic development has expanded significantly beyond traditional laboratory reagents to include sophisticated computational and analytical platforms. The BAITSAO model exemplifies this evolution, utilizing large language model embeddings for drugs and cell lines to predict synergistic effects of drug combinations [101]. This approach generates context-enriched representations that capture functional similarities and response patterns, enabling more accurate prediction of combination therapy outcomes.
Federated learning frameworks like FedECA represent another critical tool category, enabling privacy-preserving collaborative research across institutions. These frameworks implement sophisticated statistical methods including inverse probability of treatment weighting for time-to-event outcomes without requiring data pooling [95]. The platform demonstrates equivalence to pooled analysis while maintaining compliance with stringent data protection regulations.
Discussion: Strategic Implications for Resource Allocation
Variance-Based Allocation Versus Uniform Distribution
The comparative success rates across therapeutic areas present a compelling case for variance-based allocation strategies. The data reveal substantial disparities in phase transition probabilities, with infectious disease programs demonstrating approximately 2.5-times higher overall probability of success compared to oncology programs [97]. This efficiency differential suggests that resource allocation strategies favoring therapeutic areas with established development pathways and higher success probabilities could yield greater overall R&D productivity.
However, the uniform distribution approach retains strategic value in maintaining diversified portfolios and exploring emerging therapeutic opportunities. Companies exhibiting the strongest pipeline health, including Roche, AstraZeneca, and Bristol-Myers Squibb, demonstrate balanced approaches that combine focus on high-probability areas with selective investment in novel mechanisms [97]. This balanced strategy mitigates the risk of therapeutic area concentration while maintaining exposure to potential breakthrough innovations.
Integrating Novel Methodologies into Development Strategy
The emerging methodologies discussed in this review offer opportunities to reshape success rate profiles across therapeutic areas. AI and machine learning applications show particular promise for addressing the high attrition rates in oncology by improving target validation, patient selection, and trial design [101] [100]. Federated learning approaches can enhance development efficiency across all areas by facilitating external control arms and reducing clinical trial costs [95].
The ongoing evolution of regulatory science further influences success rate dynamics. Initiatives such as the FDA's support for novel endpoints like measurable residual disease in oncology create opportunities to streamline development pathways [100]. Similarly, regulatory harmonization efforts focusing on vulnerable populations may impact development strategies for pediatric, geriatric, and rare disease populations [100].
This comparative review demonstrates substantial heterogeneity in success rates across therapeutic areas, with infectious disease programs exhibiting the highest probability of success and oncology programs facing the most significant development challenges. These differential success rates provide strong support for variance-based allocation strategies that prioritize resources toward therapeutic areas with more established development pathways and higher success probabilities.
However, the rapid evolution of drug development methodologies is dynamically reshaping these probability landscapes. Artificial intelligence, federated learning, risk-based approaches, and endpoint innovation collectively offer opportunities to enhance success rates across all therapeutic areas. The organizations most likely to succeed in this evolving landscape will be those that strategically balance variance-based resource allocation with selective investments in novel methodologies and emerging therapeutic opportunities.
The future of pharmaceutical development will increasingly depend on sophisticated portfolio management strategies that integrate historical success rate data with forward-looking assessments of methodological innovations. This integrated approach will enable researchers, scientists, and drug development professionals to optimize resource allocation while advancing therapeutic innovations across the disease spectrum.
Conclusion
The strategic implementation of variance-based allocation presents a paradigm shift from traditional uniform distribution, offering a powerful tool to enhance the efficiency and success of clinical research. Empirical evidence confirms that variance-based methods can preserve statistical power even under model misspecification, optimize resource use under budgetary constraints, and adapt to complex modern trial designs like platform trials. While challenges such as low enrollment and ethical considerations remain, the integration of these methods with MIDD, federated learning, and adaptive designs points toward a more efficient future for drug development. Future directions should focus on standardizing these methodologies across regulatory agencies, expanding their application in rare diseases, and further exploring AI-driven optimization to accelerate the delivery of new therapies to patients.
References
- 1. Variance of Uniform Distribution - Formula, Proof, and ... [https://mathmonks.com/standard-deviation/variance-of-uniform-distribution]
- 2. Probability distribution [https://en.wikipedia.org/wiki/Probability_distribution]
- 3. Equipoise and the ethics of clinical research [https://pubmed.ncbi.nlm.nih.gov/3600702/]
- 4. Clinical equipoise [https://en.wikipedia.org/wiki/Clinical_equipoise]
- 5. Random treatment assignment using mathematical equipoise ... [https://pubmed.ncbi.nlm.nih.gov/21348950/]
- 6. Optimizing Shot Assignment in Variational Quantum ... [https://arxiv.org/html/2307.06504v2]
- 7. What do we talk about when we talk about “equipoise ... - Trials [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-023-07221-3]
- 8. A New Generalization of the Uniform Distribution [https://www.mdpi.com/2227-7390/12/15/2328]
- 9. OPTIMUM TREATMENT ALLOCATION RULES UNDER A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3832358/]
- 10. Mean-Variance Optimization – an Overview - CFA, FRM ... [https://analystprep.com/study-notes/cfa-level-iii/mean-variance-optimization-an-overview/]
- 11. The benefits of differential variance-based constraints in ... [https://www.sciencedirect.com/science/article/abs/pii/S0377221713003172]
- 12. Shot-Efficient ADAPT-VQE via Reused Pauli ... [https://arxiv.org/html/2507.16879v1]
- 13. a spatial statistical study based on two cross-sectional ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1604008/full]
- 14. Statistical inference and optimal design for step-stress ... [https://www.sciencedirect.com/science/article/pii/S0951832025007069]
- 15. Randomization in the age of platform trials [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02693-0]
- 16. An overview of platform trials with a checklist for clinical ... [https://www.sciencedirect.com/science/article/pii/S0895435619309874]
- 17. Optimal allocation strategies in platform trials with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11041082/]
- 18. Efficient stage-wise allocation ratios in multi-arm ... [https://www.sciencedirect.com/science/article/pii/S1551714425001028]
- 19. Operating characteristics of unequal allocation ratios in ... [https://www.sciencedirect.com/science/article/pii/S2451865425000249]
- 20. The net effect of alternative allocation ratios on recruitment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2864093/]
- 21. Operating characteristics of unequal allocation ratios in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11889599/]
- 22. Optimal placebo-treatment comparisons in trials with an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10118159/]
- 23. Practical Considerations for Demonstrating Drug ... [https://www.biopharminternational.com/view/practical-considerations-demonstrating-drug-substance-uniformity]
- 24. The biggest challenges clinical trials will face in 2025 [https://www.clinicaltrialsarena.com/features/clinical-trials-challenges-expect-2025/]
- 25. Uniform distribution of drug: Significance and symbolism [https://www.wisdomlib.org/concept/uniform-distribution-of-drug]
- 26. High Concentrations of Drug in Target Tissues Following ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4646071/]
- 27. Optimal Allocation of Research Funds under a Budget ... [https://pubmed.ncbi.nlm.nih.gov/32845233/]
- 28. Optimal Allocation of Sample Sizes to Multicenter Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC3694743/]
- 29. Alzheimer's disease drug development pipeline: 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131090/]
- 30. An End-to-End Framework for Marketing Effectiveness ... [https://arxiv.org/abs/2302.04477]
- 31. [2304.03035] Optimal allocation strategies in platform trials [https://arxiv.org/abs/2304.03035]
- 32. Optimal allocation strategies in platform trials with ... [https://pubmed.ncbi.nlm.nih.gov/38505941/]
- 33. Heterogeneity of Variance - Sage Research Methods [https://methods.sagepub.com/ency/edvol/the-sage-encyclopedia-of-communication-research-methods/chpt/heterogeneity-variance]
- 34. Chapter 6 - Multilevel Model with Heterogeneous for... Variance [https://quantdev.ssri.psu.edu/sites/qdev/files/ILD_Ch06_2017_MLMwithHeterogeneousVariance.html]
- 35. Modelling heterogeneity variances in multiple treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3554418/]
- 36. Statistical Methods for Quantifying Between-study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7901832/]
- 37. How to quantify between-study heterogeneity in single-arm ... [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-025-02831-1]
- 38. Advancing drug development with “Fit-for-Purpose†modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 39. Advanced Methods for Dose and Regimen Finding During ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5529745/]
- 40. Three steps toward dose optimization for oncology ... [https://www.sciencedirect.com/science/article/pii/S2451865424000760]
- 41. Model-Informed Drug Development Paired Meeting Program [https://www.fda.gov/drugs/development-resources/model-informed-drug-development-paired-meeting-program]
- 42. Application of Model-Informed Drug Development in Dose ... [https://pubmed.ncbi.nlm.nih.gov/38426370/]
- 43. CERTAINTY 2025: The power of Model-Informed Drug ... [https://www.certara.com/blog/certainty-the-power-of-model-informed-drug-development/]
- 44. Model-Informed Precision Dosing [https://en.wikipedia.org/wiki/Model-Informed_Precision_Dosing]
- 45. Advances in machine learning for optimizing ... [https://www.sciencedirect.com/science/article/pii/S1570164625000153]
- 46. The Pivotal Role of AI in Clinical Trials: From Digital Twins ... [https://www.biopharmatrend.com/artificial-intelligence/the-pivotal-role-of-ai-in-clinical-trials-from-digital-twins-to-synthetic-control-arms-176/]
- 47. Adaptive Trial Design: A Guide to Flexible Clinical Trials [https://intuitionlabs.ai/articles/adaptive-clinical-trial-design]
- 48. Synthetic control arms: full impact yet to be realised [https://www.clinicaltrialsarena.com/interviews/synthetic-control-arms-full-impact-yet-to-be-realised/]
- 49. Synthetic control arm from mixed clinical trials and real-world ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583804/]
- 50. 2025 Trends: Leveraging Real-World Data for Synthetic ... [https://www.appliedclinicaltrialsonline.com/view/2025-trends-leveraging-real-world-data-synthetic-control-arms]
- 51. The What, Why and How of Adaptive Clinical Trials [https://www.quanticate.com/blog/what-why-how-adaptive-clinical-trials]
- 52. Can you trust clinical trial design software? Top solutions in ... [https://clinicaltrialrisk.org/clinical-trial-protocol-software/can-you-trust-clinical-trial-design-software-top-solutions/]
- 53. Top Electronic Data Capture (EDC) Systems for Clinical ... [https://ccrps.org/clinical-research-blog/directory-of-electronic-data-capture-edc-systems-for-clinical-trials]
- 54. Value-adaptive clinical trial designs for efficient delivery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12139198/]
- 55. 5 Ways to Improve Patient Recruitment in Clinical Trials 2025 [https://www.patiro.com/insights/5-ways-to-improve-patient-recruitment-in-clinical-trials-in-2025]
- 56. Fast Enrollment: A Strategic Solution for Increasing the ... [https://acrpnet.org/2025/04/08/fast-enrollment-a-strategic-solution-for-increasing-the-negotiating-power-of-clinical-sites]
- 57. 5 ways to make patient enrollment in clinical trials easier [https://www.antidote.me/blog/5-ways-to-make-patient-enrollment-easier]
- 58. mortality effects, uncertainty, and informed consent [https://pmc.ncbi.nlm.nih.gov/articles/PMC6726291/]
- 59. Bayesian model averaging for mortality forecasting using ... [https://www.sciencedirect.com/science/article/abs/pii/S0169207022000243]
- 60. The effect of pharmaceutical innovation on longevity [https://www.sciencedirect.com/science/article/pii/S1570677X2200020X]
- 61. Mortality: a statistical approach to detect model ... [https://ideas.repec.org/p/hal/journl/hal-01149396.html]
- 62. Mortality Risk Prediction Models for People With Kidney ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11699530/]
- 63. Statistical Power: Definition, Formula & Practical Guide to ... [https://www.mida.so/blog/statistical-power]
- 64. Ethical considerations in the design, execution, and analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6749924/]
- 65. Finding the right power balance: Better study design and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10773938/]
- 66. A comparison of allocation strategies for optimising clinical ... [https://www.sciencedirect.com/science/article/pii/S0167947322001396]
- 67. Ethical Guidelines for Statistical Practice [https://www.amstat.org/your-career/ethical-guidelines-for-statistical-practice]
- 68. Group allocation (stratification) [https://www.xltoolbox.net/allocate.html]
- 69. Optimizing Treatment Allocation in Randomized Clinical Trials ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10843680/]
- 70. The evolution of data ethics in clinical research and drug ... [https://www.sciencedirect.com/science/article/pii/S2352552520300554]
- 71. Optimal contrast analysis with heterogeneous variances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6435144/]
- 72. Drug-development, dose-selection, rational combinations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8169070/]
- 73. Demystifying Cost-Efficiency in LLM Serving over ... [https://openreview.net/forum?id=xnEv5pq4cB¬eId=C5oC5Gtx8F]
- 74. Multi-Heterogeneous Renewable Energy Scheduling ... [https://www.sciencedirect.com/science/article/abs/pii/S2210537925000940]
- 75. Accounting for cost heterogeneity on the demand in ... [https://www.sciencedirect.com/science/article/abs/pii/S0377221720304094]
- 76. Federated learning in healthcare: Transformative 2025 [https://lifebit.ai/blog/federated-learning-in-healthcare/]
- 77. Federated Learning in 2025: What You Need to Know [https://dev.to/lofcz/federated-learning-in-2025-what-you-need-to-know-3k2j]
- 78. Federated Learning: The Future of Privacy-Preserving AI in ... [https://medium.com/ai-explorerz/federated-learning-the-future-of-privacy-preserving-ai-in-2025-9f9a8c931265]
- 79. FedUV: Uniformity and Variance for Heterogeneous ... [https://arxiv.org/abs/2402.18372]
- 80. Towards a Larger Model via One-Shot Federated Learning ... [https://arxiv.org/html/2508.13625v1]
- 81. Federated Learning for ADMET Prediction [https://www.apheris.com/resources/blog/federated-learning-for-admet-prediction-expanding-model-applicability]
- 82. Federated learning: a privacy-preserving approach to data- ... [https://www.frontiersin.org/journals/drug-safety-and-regulation/articles/10.3389/fdsfr.2025.1579922/full]
- 83. Towards one-shot federated learning: Advances, ... [https://www.sciencedirect.com/science/article/pii/S0925231225027602]
- 84. Variance: Examining Variance in Uniform Distribution [https://fastercapital.com/content/Variance--Examining-Variance-in-Uniform-Distribution--An-In-Depth-Analysis.html]
- 85. Distributing Quantum Computations, Shot-Wise [https://www.mdpi.com/1999-5903/17/11/507]
- 86. Quantifying individual-level heterogeneity in infectiousness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10594662/]
- 87. A Comparison of Techniques for Creating Permuted ... [https://www.appliedclinicaltrialsonline.com/view/comparison-techniques-creating-permuted-blocked-randomization-lists]
- 88. Trends and disparities in the research and development of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599347/]
- 89. Emerging and reemerging infectious diseases [https://www.nature.com/articles/s41392-024-01917-x]
- 90. Optimal allocation to treatment sequences in individually ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10262341/]
- 91. Variance-based sensitivity analysis of tuberculosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9682306/]
- 92. Computational tools and data integration to accelerate ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1502484/full]
- 93. Better Benchmarking Improves Drug Development ... [https://www.intelligencia.ai/better-benchmarking-elevates-pharma-decision-making/]
- 94. Polaris - The benchmarking platform for drug discovery [https://polarishub.io/]
- 95. FedECA: federated external control arms for causal ... [https://www.nature.com/articles/s41467-025-62525-z]
- 96. Comparative efficacy and safety of second-line therapies ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1697949/full]
- 97. Who's Winning the Pharmaceutical R&D Pipeline Race in ... [https://www.ozmosi.com/pharmaceutical-rd-pipeline-race-2025/]
- 98. Comparative long-term outcomes of first-line CDK4/6 ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1600892/full]
- 99. A Comparative Review of the Pharmacology of Dalbavancin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12480267/]
- 100. New Predictions for 2025 [https://globalforum.diaglobal.org/issue/january-2025/additional-predictions-for-2025/]
- 101. Building a unified model for drug synergy analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12081637/]
- 102. 2025 Clinical Data Trend Report [https://www.veeva.com/2025-clinical-data-trend-report/]